Bristol research leads to a worldwide fall in the number of cot deaths.
Submitting Institution
University of BristolUnit of Assessment
Public Health, Health Services and Primary CareSummary Impact Type
HealthResearch Subject Area(s)
Medical and Health Sciences: Paediatrics and Reproductive Medicine, Public Health and Health Services
Summary of the impact
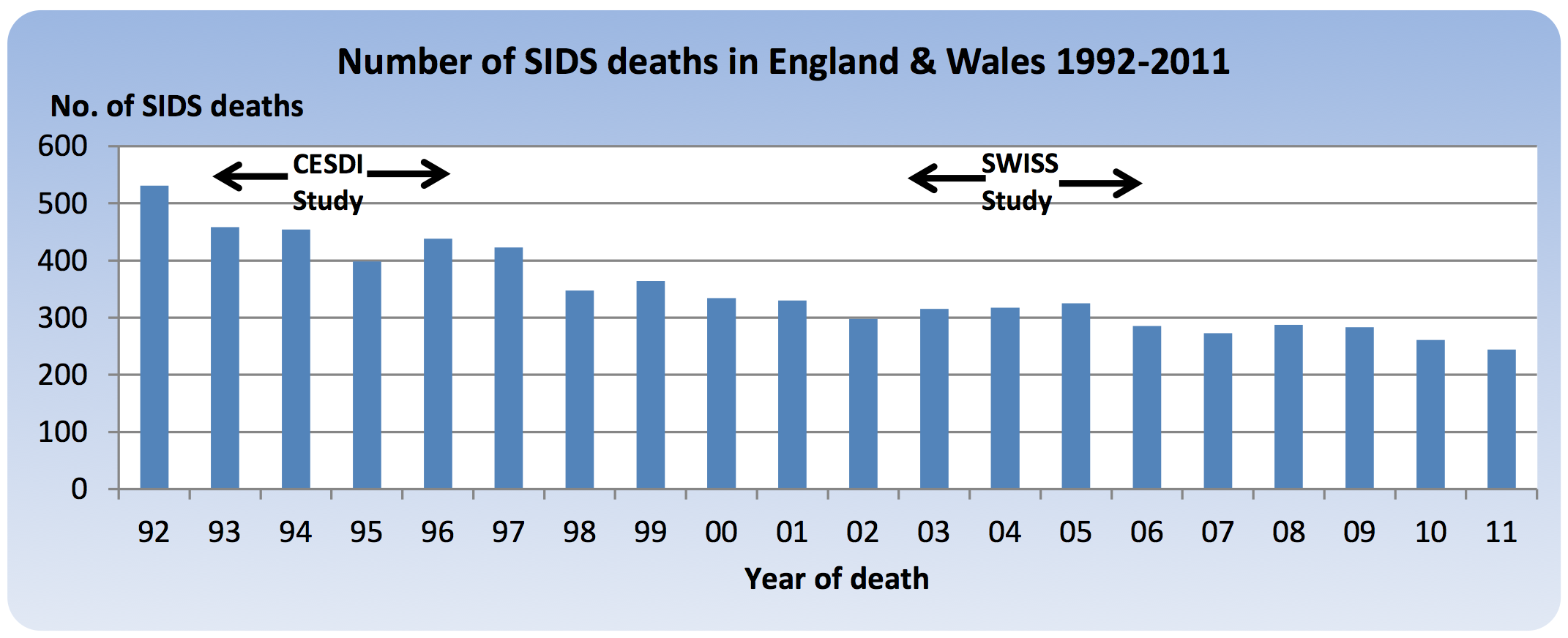
University of Bristol research has led to a marked and persisting
reduction in the number of cot deaths (sudden infant death syndrome or
SIDS). The dramatic 67% fall from 1988 to 1992 in England and Wales
resulted from the identification of risks associated with putting babies
to sleep face-down (prone). Nationally, death rates have more than halved
again (54% fall) between from 1992 and 2011, with an estimated additional
1025 lives saved between 2008 and 2011, after two studies conducted in
1993-6 and 2003-6 identified further contributory risk factors. Tens of
thousands of SIDS deaths worldwide have been prevented thanks to the
team's research, international collaboration and development of
risk-reduction recommendations.
Underpinning research
University of Bristol (UoB) led studies, published in the early 1990s
were the first population-based investigations to document the importance
of a number of factors (prone sleeping position, wrapping infants too
warmly and pre-natal smoking) that contribute to SIDS. Subsequently, two
case-control studies were conducted by Peter Fleming (Professor of Infant
Health and Developmental Physiology, UoB since 1982) and Peter Blair
(Senior Research Fellow, UoB since 1992). Data from the Confidential
Enquiry into Stillbirths and Deaths in Infancy (CESDI) in 1993-6 [1-3] and
the South West Infant Sleep Scene (SWISS) study in 2003-6 [4] identified a
number of further contributory factors to deaths. These included
post-natal smoking, parental drug and alcohol use when bed-sharing,
co-sleeping on a sofa, putting the baby to sleep on their side and loose
covering found over the infant's head. The team also identified factors
not contributory to the risk of SIDS (e.g. immunisation and toxic gas
emanating from mattresses) and some that were beneficial (e.g. infants
sleeping in the same room as parents, dummy use and breastfeeding). Advice
against the prone sleeping position had already been widely adopted prior
to CESDI in 1993-6. In the ten years between CESDI and SWISS, prone
sleeping position rates did not change, but rates of infants being placed
on their side to sleep, infants exposed to tobacco smoke after the birth
and infants found with bedding over their heads decreased while rates of
infants being placed `feet to foot' (with their feet at the foot of the
cot to avoid wriggling under the covers) and infants being breastfed
increased suggesting that the subsequent 54% fall in SIDS rates was
related to the further contributory factors identified by the UoB team
(see table below). [4]
| Impact
of risk reduction advice in the 10 years between CESDI and SWISS
studies |
| Risk(R) or Protective(P) Factor |
CESDI
Study
Fleming & Blair 1993-6[1] |
SWISS
study
Blair & Fleming 2003-6[3] |
|
SIDS% |
Controls% |
SIDS% |
Controls% |
| R-Placed prone to sleep |
15% |
3% |
14% |
6% |
| R-Placed on side to sleep |
41% |
28% |
18% |
10% |
| R-Postnatal exposure to smoke |
54% |
23% |
16% |
6% |
| R-Head covered by bedding |
16% |
3% |
5% |
0% |
| P-Feet placed at foot of cot |
3% |
4% |
50% |
60% |
| P-Mother attempted to breastfeed |
44% |
60% |
70% |
79% |
Evidence from these two population-based, case-control studies ten years
apart suggests that the messages from the UoB team have changed parental
behaviour. Laboratory and community studies of thermal balance (solely
conducted in Bristol) have led to detailed recommendations in current
safety guidelines regarding how much bedding infants should have,
according to bedroom temperature.[4, 5] In the last five years the team
has identified potential risks to the baby if they share the same sleep
surface and have been working with UNICEF to provide a more evidence-based
approach that acknowledges the importance of breastfeeding while outlining
specific hazards when bed-sharing deaths occur.
UoB-led studies in the Avon Longitudinal Study of Parents and Children
(ALSPAC) study showed no adverse effects from changes in sleeping position
advice and findings published in 2010 suggest an interdependent effect
with bed-sharing and breastfeeding.[6]
The UoB team also includes PJ Berry (Pathologist 1983-2001), P Sidebotham
(Sen Clinical Lecturer 1997-2005) and J Golding (Prof of Paediatric &
Perinatal Epidemiology 1985-present).
References to the research
[1] Fleming PJ, Blair PS, Bacon C et al. Environment of infants during
sleep and risk of the sudden infant death syndrome: results from 1993-5
case-control study for confidential inquiry into stillbirths and deaths in
infancy. BMJ 1996; 313:191-5 (Document can be supplied upon
request)
[2] Blair PS, Fleming PJ et al. Smoking and the sudden infant death
syndrome: results from 1993-5 case-control study for confidential inquiry
into stillbirths and deaths in infancy. BMJ 1996; 313:195-8.
(Document can be supplied upon request)
[3] Blair PS, Fleming PJ, Smith IJ et al. Babies sleeping with parents:
case-control study of factors influencing the risk of sudden infant death
syndrome. BMJ 1999;319:1457-61. (Document can be supplied upon
request)
[4] Blair PS, Sidebotham P, Evason-Coombe C, Edmonds M, Heckstall-Smith
EM, Fleming P. Hazardous cosleeping environments and risk factors amenable
to change: case-control study of SIDS in south west England. BMJ
2009;339:b3666. DOI:10.1136/bmj.b3666
[5] Blair PS, Sidebotham P, Berry PJ, et al. Major epidemiological
changes in sudden infant death syndrome: a 20-year population-based study
in the UK. Lancet 2006;367:314-9. DOI:
10.1016/SO140-6736(06)67968-3
[6] Blair
PS, Heron
J, Fleming
PJ. Relationship between bed sharing and breastfeeding:
longitudinal, population-based analysis. Pediatrics
2010; 126(5):e1119-26.
DOI:10.1542/peds.2010-1277
Peer reviewed grants: UK Department of Health £620,000 (1993-8); FSID
Charity £80,580 (1995-6); Babes in Arms Charity £109,500 (2000-6) and
Charitable Trusts for UoB £54,000 (2006-7).
Details of the impact
Implementation in the UK of SIDS risk reduction programmes based on UoB
research findings was followed by a 67% fall in SIDS rates by 1992; the
number of SIDS deaths in England and Wales fell from 1597 in 1988 (2.3
deaths per 1000 live births) to 531 in 1992 (0.77 per 1000 live births).
As the Figure below shows, the number of deaths fell by a further 54% to
244 by 2011 (0.34 per 1000 live births), the last year for which national
data is available.
 Publication dates (number of studies): ‘CESDI’ study - 1995(1), 1996(2), 1999(3), 2000(3), 2001(1), 2002(2), 2003(2), 2004(2), 2006(3) and 2007(1). ‘SWISS’ study - 2009(1) and 2010(1).
Publication dates (number of studies): ‘CESDI’ study - 1995(1), 1996(2), 1999(3), 2000(3), 2001(1), 2002(2), 2003(2), 2004(2), 2006(3) and 2007(1). ‘SWISS’ study - 2009(1) and 2010(1).
This further fall was not due to any change in prone positioning in
England but concomitant with changes in other identified risk factors (see
Table in Section 2).
If death rates had remained the same as 1992 over 10,000 infants would
have died in England and Wales between 1993 and 2011 rather than the 6434
SIDS deaths that did occur. Over 2,100 would have died from 2008 to 2011
rather than the 1075 deaths that did occur. The persistent year on year
fall in SIDS rates over the last two decades has been instrumental in the
halving of the post-neonatal infant mortality rate in England and Wales
over the same time period (from 2.2 deaths to 1.2 deaths per 1000 live
births).
At every stage of this process the UoB researchers have been closely
involved: generating the findings; developing the risk-reduction messages;
changing statutory law in 2008 on how child deaths are investigated (see
below); and collaborating with national and international organisations to
ensure families are given accurate information to care for their infants
in ways that lead to the lowest possible risk of SIDS. In the last 5 years
they have been particularly involved in the translational work of getting
their evidence-based findings implemented into public health policy.
In UK [a] and Australian [b] parent information leaflets, every
recommendation to reduce the risk of SIDS is based partly or fully on the
results of the UoB studies. Collaborative work with other groups in
Germany, New Zealand, and Scandinavia has led to the development of
standardised protocols for data collection in the investigation of
unexpected infant deaths, which in turn have allowed more rapid
identification and evaluation of significant changes in parenting
practices and their effects.
UoB studies on infant thermal balance have produced charts of optimal
thermal conditions adopted by both manufacturers and parents in many
countries, and sequential studies show a clear reduction in covering
(infant clothes and bedding combined) from an average of 8 tog (unit of
thermal resistance) 20 years ago to just 2.4 tog more recently.[4 — page
8]
Fleming and Blair recognise that findings from their studies need to fit
with current evidence of infant care practices outside the field of SIDS
so that consistent public health messages can be given to parents and
health professionals. They have worked closely in the last five years with
UNICEF UK [c, d], who are currently promoting breastfeeding in Baby
Friendly Hospitals, to produce a leaflet `Caring for your baby at night'
which encourages breastfeeding, acknowledges some parents may want to
bed-share but outlines the circumstances in which bed-sharing may be
unsafe. An evidence-based guideline for health professionals [e, f]
accompanies the leaflet (lead author Blair). The leaflets and guidelines,
printed in January 2012, have proved popular — over 210,000 have so far
been distributed, mainly to NHS hospitals, trusts and health visiting
teams. Blair is a regular invited speaker at health care professional
conferences and seminars (see a selection of UK and International lectures
since 2008 [g, h, i]) to promote the UoB-based findings.
The UoB approach to the investigation of unexpected infant deaths and the
care of families was adopted by the Kennedy Committee which was set up by
the Royal College of Pathologists and Royal College of Paediatrics and
Child Health to improve the quality of such investigations after a series
of miscarriages of justice in 2003, and was subsequently incorporated into
the Children Act 2004, becoming a statutory requirement throughout England
from 2008. This process of child death reviews (in which Fleming was
centrally involved) has led to a major change in the way medico-legal
agencies involved in providing services to children interact, with a
resultant improvement in the quality of such investigations and services
to bereaved families.[j, k]
Fleming was elected as Vice Chair of the International Society for the
Study and prevention of Perinatal and Infant Deaths (ISPID) in 2008,
succeeded in that role in 2010 by Blair. The Society is instrumental in
the delivery of SIDS public health campaigns in different countries. Both
have been involved in developing risk reduction messages on the ISPID
website (http://www.ispid.org/) which
receives around 300 visits a day. Blair currently helps co-ordinate the
website activities and chairs the epidemiology group working towards
consensus positional statements on safe infant care practices. Both
researchers have worked extensively on the development of internationally
agreed policies for parent education and support, and on advice about
parenting practices, which have been adopted in many countries.
In 2006 Fleming was included in the "Eureka UK" publication celebrating
the 100 most important research achievements of British Universities. In
2009 Blair was awarded an Honorary Fellowship by UNICEF for work in the
SIDS field and in 2012 both Fleming and Blair were awarded the UoB
Vice-Chancellor Impact award for their translational research in this
field. This work has also been instrumental in the UoB receiving the
Queen's anniversary prize for Higher and Further Education in the field of
Obstetrics and Neonatal practice in 2012-14.[l]
Sources to corroborate the impact
[a] http://www.lullabytrust.org.uk/document.doc?id=300
UK (FSID now Lullaby Trust). Evidence base for risk reduction messages,
PJF and PSB work cited 15 times
[b] http://www.sidsandkids.org/wp-content/uploads/SidsSafeSleeping14ppa1.pdf
Australian SIDS and Kids leaflet. PSB and PJF acknowledged for their work
on the last page
[c] Letter of support from Sue Ashmore, Programme Director, UNICEF UK
Baby Friendly Initiative
[d] http://www.unicef.org.uk/BabyFriendly/News-and-Research/Research/Cot-death/Study-draws-link-between-increased-risk-of-SIDS-and-alcohol-or-drug-use-when-co-sleeping/
and
http://www.unicef.org.uk/BabyFriendly/News-and-Research/Research/Cot-death/Research-concludes-no-increase-in-risk-of-cot-death-from-bed-sharing-for-infants-over-14-weeks-with-non-smoking-parents/
Exemplars of involvement with UNICEF UK including website reporting
research conducted by PJF and PSB regarding both the hazards of
bed-sharing and when bed-sharing is safe.
[e] http://www.unicef.org.uk/BabyFriendly/Resources/Resources-for-parents/Caring-for-your-baby-at-night/
Caring for your baby at night leaflet: (UNICEF 2012) both PJF and PSB were
instrumental in advising on the contents of this leaflet.
[f]http://www.unicef.org.uk/Documents/Baby_Friendly/Leaflets/HPs_Guide_to_Coping_At_Night_Final.pdf
Health profession guidelines to the UNICEF leaflet. PSB is the lead
author.
[g] http://www.unicef.org.uk/Documents/Baby_Friendly/Programmes/3/08programme.pdf
PSB gives talk to 500 health professionals in Glasgow 2008, Page 3,
abstract page 8 of programme.
[h] https://www.dur.ac.uk/sleep.lab/sim/
PSB gives talk in Durham, 2012, similar talks given in Bristol 2012 and
2013.
[i] Flyer listing a series of seminars delivered to health professionals
in Australia (program 2: Sydney, Adelaide and Perth) in 2012 by PSB
[j] http://www.rcpath.org/publications-media/publications/sudden-unexpected-death-in-infancy
The Kennedy Report. PJF was a member of the committee that wrote this
report and helped write chapter 7, on investigating childhood deaths.
[k]http://www.education.gov.uk/childrenandyoungpeople/safeguardingchildren/childdeathreview/a0068831/why-jason-died-a-dvd-familiarisation-resource
A DVD: "Working together to safeguard children" 2010. PJF is featured
extensively in the accompanying DVD.
[l] Letter of award to UoB for the Queen's Anniversary Prizes for Higher
and Further Education for 2012-14 (Obstetrics and Neonatal Practice-Saving
Babies lives around the world).