Submitting Institution
University of CambridgeUnit of Assessment
Geography, Environmental Studies and ArchaeologySummary Impact Type
SocietalResearch Subject Area(s)
Medical and Health Sciences: Public Health and Health Services
Summary of the impact
Tucker's ethnographic research on the social worlds inhabited by
township `Men who have Sex with Men' (MSM), and his quantitative analysis
of the associations between social and psycho- social conditions and risky
sexual practices for such men, led to the development of the innovative
Ukwazana HIV prevention programme — the first of its kind in Africa.
Ukwazana, meaning `getting to know each other' in isiXhosa, is based
across the central townships of Cape Town, and is unique in fostering
partnerships with marginalised township MSM, engaging them collaboratively
in HIV prevention initiatives. Based on Tucker's research findings, it is
the first scheme to recognise, and tackle, social and psychosocial factors
such as homophobia, depression and loss of self- esteem, which often
result in risky sexual practices and related illnesses among MSM. This new
approach was timely since, despite numerous previous HIV prevention
campaigns aimed at township MSM, HIV prevalence for this group was three
times the national average.
Underpinning research
The underpinning research, conducted by Dr Andrew Tucker in the
Department of Geography, University of Cambridge (ESRC Research Fellow,
Sept. 2006 - Oct 2007; University Lecturer, 2008-), involved two main
projects: an ESRC Postdoctoral Fellowship (the `Fellowship') and a project
funded by the Anova Health Institute of South Africa, 2010-2013 (the
`Anova Project'). Both projects broke new ground.
The Fellowship showed how men with same-sex desire, from different
`racially-defined' communities in Cape Town (`white', `coloured' and
`black African'), encountered distinctive forms of heteronormative
regulation within their own social spaces, which shaped how open and safe
they could be about their sexuality. The Fellowship, which involved
substantial further development of earlier research for a PhD, facilitated
new fieldwork in South Africa, produced the novel conceptual frame of
`queer visibilities', and led ultimately to the publication of a monograph
with the same title (see Section 3.i) and two journal articles (see 3.ii
and 3.iii). The new framing attended to the interplay and political
significance of varying forms of non-heteronormative visibility in the
urban environment. One important conclusion reached by the research was
that Western notions of `the closet' as a form of secrecy about sexual
identity did not necessarily hold for communities of men historically less
rigidly defined by heterosexual/homosexual binaries. This in turn meant
that men from different communities often had vastly different sexual and
gender identity categories, social networks, community structures and ways
of safely negotiating urban space. The research therefore judged Western
ideas of sexual political liberation or health service provision as
potentially inappropriate for communities with different heteronormative
histories. In relation specifically to health and HIV prevention, the
research suggested that MSM in black African township communities had
historically been poorly served by the Western-centric health
organisations tasked to assist them, in part as a result of assumed
congruity and affiliation with Western notions of `gay' identity. This had
led to feelings of mistrust and disinterest among black African MSM
towards health NGOs and their programmes.
The subsequent Anova Project focused on developing and tailoring a new
style of HIV prevention programme, based on sustained MSM community
engagement, in the former townships of Cape Town. While research elsewhere
had highlighted the potential efficacy of deploying community- based HIV
prevention programmes (e.g. Campbell 2003), none had been undertaken
previously for black African MSM anywhere in Africa. The Anova Project
therefore deployed one of the largest quantitative surveys ever undertaken
in Africa in order to understand how social and psycho-social factors
operating at the community-scale might be associated with riskier sexual
behaviour (see 3.v and 3.vi). Though they had not traditionally been seen
as important in HIV prevention for MSM, factors such as homophobia,
depression and low self-efficacy were found to be central to the
successful assistance of MSM in HIV risk reduction. Drawing on the
Fellowship, the Anova Project was also able to further explore the
specific geographical reach of these unique social and psycho- social
pathways to HIV risk. For example, key sites of homophobic stigma (the
local `shebeen' or informal tavern) proved to be significant, and
particular to township MSM, due to the lack of any form of demarcated
social `gay spaces'.
Finally, the research element of this project devoted considerable effort
to overcome feelings of mistrust and disinterest on the part of township
MSM towards health organisations, highlighted during the Fellowship.
Qualitative methods including interviews and focus groups during the Anova
Project explored how best to work with MSM volunteers and also how to make
them feel valued and protected by the organisation (see 3.iv). The Anova
Project coincided with, and fed into, the development of the Ukwazana HIV
prevention programme, meeting the need to find ways of maintaining
community interest in the Ukwazana programme and hence offsetting the
problems of limited or sporadic community engagement highlighted by the
Fellowship.
References to the research
i. Tucker, A., 2009. Queer visibilities: Space, Identity and
Interaction in Cape Town. RGS/IGB book series. Chichester:
Wiley-Blackwell
ii. Tucker, A., 2010. 'The 'rights' (and 'wrongs') of articulating race
with sexuality: the conflicting nature of hegemonic legitimisation in
South African queer politics' Social & Cultural Geography
11(5), 433-449
iii. Tucker, A., 2010. 'Shifting boundaries of sexual identities: the
appropriation and malleability of 'gay' in South African township spaces'
Urban Forum 21(2), 107-122
iv. Tucker, A., de Swardt, G., Struthers, H., McIntyre, J. 2013.
`Understanding the needs of Men who have Sex with Men (MSM) health
outreach workers: exploring the interplay between volunteer training,
social capital and critical consciousness' AIDS and Behaviour
17(Supp 1), S33-S42
v. Tucker, A., Liht, J., de Swardt, G., Jobson, G., Rebe, K., Struthers,
H., McIntyre, J., 2013. `An exploration into the role of depression and
self-efficacy on township Men who have Sex with Men's ability to engage in
safer-sexual practices' AIDS Care http://dx.doi.org/10.1080/09540121.2013.764383
vi. Tucker, A., Liht, J., de Swardt, G., Jobson, G., Rebe, K., McIntyre,
J., Struthers, H., 2013. `Homophobic stigma, depression, self-efficacy and
Unprotected Anal Intercourse (UAI) for peri-urban township Men who have
Sex with Men (MSM) in Cape Town, South Africa: A cross-sectional
association model' AIDS Care doi: 10.1080/09540121.2013.859652
Research Grants:
ESRC Research Fellowship — `Male homosexual visibility in Cape Town'; PI:
Dr Andrew Tucker; October 2006 — September 2007; £63,854
Anova Health Institute — `MSM Ecosystem'; PI: Dr Andrew Tucker; October
2010 — September 2013; £56,419
Details of the impact
The Ukwazana HIV-prevention scheme was the first programme of its kind in
Africa, and the first to commit to long-term engagement with township MSM,
whereby the men themselves helped steer the course of HIV community
interventions. Tucker's Fellowship and Anova Research Project had direct
impact on the ways in which the Anova Health Institute, through their
Health4Men subsidiary project in the Cape Town townships, designed,
structured and implemented the Ukwazana Programme. Tucker's involvement as
a Consultant for the Anova Health Project enabled his research findings to
directly shape how the Ukwazana programme developed and functioned. In
particular, it was as a result of the projects outlined in Section 2, that
Ukwazana focused heavily on MSM community engagement and empowerment, and
on the need to address social and psycho- social factors associated with
sexual risk-taking behaviour among township MSM. The Ukwazana Programme's
interventions, exemplified below, clearly illustrate the impact of Dr
Tucker's research:
1. Reflexive engagement. Research during the Fellowship
had highlighted the need to move away from more traditional and
unsuccessful didactic methods of interfacing with township MSM, which did
not consider the specific needs of this group. The Ukwazana programme
therefore had to involve continual evaluation of the programme itself by
township MSM. As such the programme was focused on a reflexive engagement
with those it was tasked to assist. This established a nuanced means of
engaging with outreach volunteers and those who attended various
activities associated with the programme. In showing how volunteers came
to understand their engagement with Ukwazana, research in the Anova
Project helped shape the approach of programme facilitators in working
with the community. It led directly, for example, to the decision to
implement specific training and workshops for volunteers and the wider
township community of MSM. Glenn de Swardt, Programme Manager Health4Men
writes `the way the program engaged with and developed collaborative
working relationships with volunteer outreach workers was impacted upon by
the research Dr Tucker undertook' (see 5.1, and Plate 1).
 Plate 1. Tucker with Ukwazana Volunteer outreach workers at Shebeen event
Plate 1. Tucker with Ukwazana Volunteer outreach workers at Shebeen event
2. Psycho-social intervention. Ukwazana also broke new
ground in Africa in attempting to engage directly with the social and
psycho-social issues that affected the likelihood of MSM engaging in
safer-sexual practices. This approach was adopted as a direct result of
Tucker's research for the Fellowship and the Anova Project, which
highlighted the under-appreciation of such factors in HIV prevention for
black African MSM. As confirmed by the Manager of the Health Project: `the
decision to focus on challenging factors such as depression, homoprejudice
and a lack of self-efficacy through the programme emerged from Dr Tucker's
research' (see 5.1). Ukwazana targeted venues such as township `shebeens'
(informal taverns), which, although frequented by township MSM, were also
known as spaces of sporadic homophobic violence. Ukwazana identified 30
such shebeens and targeted these to make them more `MSM friendly'. Key
activities included Ukwazana `launch events' where outreach workers from
Health4Men presented the Ukwazana programme to the community through an
evening of engagement activities. The outreach coordinator at Health4Men
estimated that approximately 1,700 community members participated in these
launches. Additionally, in an attempt to increase MSM community solidarity
— a form of social capital - and promote a positive image of MSM to the
wider community to help mitigate against homophobia, MSM were involved in
a number of `good causes' events termed `Men of Action'. These included
cleaning up areas of the townships and distributing food to other
disadvantaged groups (see Plate 2). A series of workshops also took place,
offering a safe space where township MSM would not simply be informed of
the need to engage in safer-sex but would also be able to discuss issues
such as homophobia, depression and a lack of self-efficacy in terms of
safer-sex. All of this constituted a significant, novel approach, derived
directly from the underpinning research.
 Plate 2 Men of Action event
Plate 2 Men of Action event
3. Innovative messaging products. In addition to the
community activities outlined above, Ukwazana developed diverse messaging
products specifically as a result of the Anova Project. Issues addressed
in this context included homophobic discrimination, low self-efficacy
(linked for example, to alcohol use and transactional sex) and the need to
engage in safer-sex. Eighteen posters were designed in collaboration with
volunteer outreach workers and displayed in locations such as shebeens,
police stations and clinics across the townships of the city. Similar
messaging regarding psycho-social concerns was also designed into drinks
coasters, 10,000 of which were disseminated to shebeens and placed on
trains. Patrons and passengers were encouraged to take coasters home.
Adverts also appeared regularly in the two main community newspapers (Vukani
and City Vision — combined distribution 500,000 per week),
highlighting forthcoming events such as Men of Action events and
workshops, and including a poster from the poster campaign. Posters were
also used as the basis for billboards (see Plate 3). Health4Men's paid
outreach workers periodically featured on the main local township radio
station, Radio Zibonele, highlighting the core aims of the
Ukwazana programme (weekly listenership of 50,000).
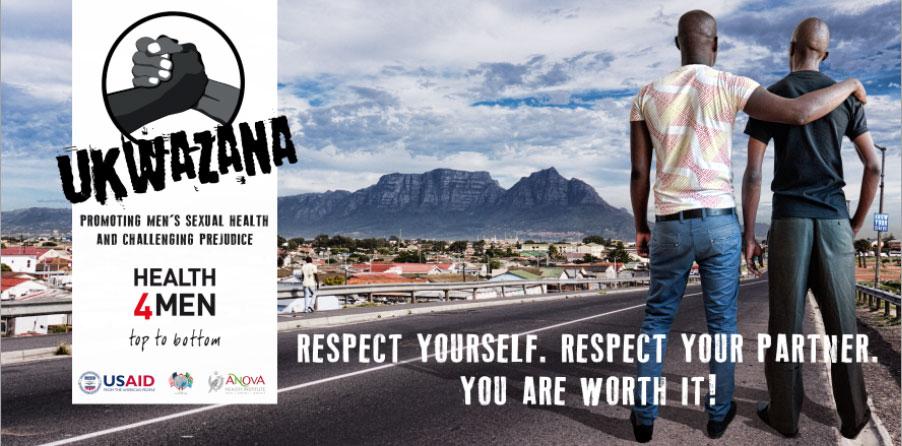 Plate 3. Ukwazana billboard (6m x 3m) placed at the main Khayelitsha
taxi-rank (July 2012 — to date). Khayelitsha is the largest township in
Cape Town, population 400,000. Source: Glenn de Swardt, Manager,
Health4Men.
Plate 3. Ukwazana billboard (6m x 3m) placed at the main Khayelitsha
taxi-rank (July 2012 — to date). Khayelitsha is the largest township in
Cape Town, population 400,000. Source: Glenn de Swardt, Manager,
Health4Men.
It is indicative of the efficacy of the programme, and of the
significance and reach of the impact of the research, that the Anova
Health Institute subsequently duplicated it in four other provinces across
South Africa (Gauteng, Mpumalanga, Limpopo and North West), starting in
2011. Given the recent timing of the interventions in Cape Town and other
provinces, it is premature to measure the impact of the Ukwazana
programme in terms of the number of lives saved or transformed sexual
practices, but the very fact that Anova decided to replicate the programme
is an indicator of the social receptivity and relevance of the
interventions.
In summary, as Helen Struthers, Chief Operating Officer of Anova,
observes, `Over several years Dr Tucker, in conjunction with the
Health4Men team in Cape Town, helped to create a variety of ways to
positively and sustainably impact on the lives of MSM. Dr Tucker's
research also influenced the ways in which Health4Men engaged with and
worked with volunteer outreach workers' (see 5.2). These interventions,
sensitively fashioned through iterative collaborations between a
researcher, practitioners, and activists, helped shape the development of
an innovative and unique approach to HIV prevention for one of the most at
risk groups in Africa.
Sources to corroborate the impact
- Letter from person 2 (Programme Manager: Health4Men, Anova Health
Institute).
- Letter from person 1 (Chief Operating Officer, Anova Health
Institute).
- Ukwazana's Facebook page detailing many of the impact activities
http://www.facebook.com/groups/249253298477550/
- An article about Ukwazana on Anova's website http://www.anovahealth.co.za/resources/entry/ukwazana_programme/
- Article from one of the foremost gay news sites in Africa highlighting
the unique nature and importance of the Ukwazana programme
http://www.mambaonline.com/article.asp?artid=5485
- A number of advertisements and articles promoting Ukwazana in township
newspapers are available in hard copy if requested.
Additional references cited:
Campbell, C., 2003. Letting them die: why HIV prevention programmes
fail. James Currey: Oxford