Understanding and addressing ethnic inequalities in mental health
Submitting Institution
Queen Mary, University of LondonUnit of Assessment
Public Health, Health Services and Primary CareSummary Impact Type
SocietalResearch Subject Area(s)
Medical and Health Sciences: Public Health and Health Services
Summary of the impact
Research by Bhui 1996-2013 showed striking differences by ethnic group in diagnosis and
management of mental health disorders due to a complex interplay of socio-cultural factors and
different perspectives of patients and professionals. Impacts included: [a] the development and
implementation of a UK-wide mental health policy 'Delivering Race Equality'; [b] a national training
and workforce development programme that shifted the conceptual paradigm from the cultural
competencies of individuals to system-wide intervention (called `cultural consultation'); [c] service
development research `Enhancing Pathways into Care' (EPIC) to implement findings and draw
lessons across four NHS Trusts; [d] incorporation of research findings into national and
international guidelines, and influence on mental health legislation and policy; and [e] a new phase
of research on implementing findings.
Underpinning research
Common mental disorders affect one in six adults in UK and cause significant morbidity. Psychotic
disorders affect one in 100 but are more disabling and have greater risk of disability, social
exclusion, self-harm, suicide and contact with specialist psychiatric services. Diagnosis and
management of mental health conditions vary by ethnicity. Since the mid-1990s Professor
Kamaldeep Bhui's team have conducted research at Queen Mary on cross-cultural psychiatry
aiming to identify and explore these ethnic differences and ensure that patients receive best care
and achieve optimum outcome whatever their ethnic group, social class, language, culture or
religion. The research can be divided into four broad groups:
2a: Descriptive epidemiology (research conducted 1996-98). Prof Bhui showed that Black
Caribbean people were more likely than Whites to enter care through forensic and psychiatric
routes, more likely to be detained under the Mental Health Act, and more likely to be diverted to
hospital from prisons, suggesting that their illness was less likely to be noticed by police or courts
[1]. His team also showed that South Asians are less likely to be referred to specialist psychiatric
care, despite seeing their GPs more often than other ethnic groups for all health problems [2].
These findings were partly, but not fully, explained by differing expressions of distress as well as
different thresholds (irrespective of GP ethnicity) for recognition of common mental disorders [2].
2b: Systematic review of compulsory detention (2001-02). A systematic review of 38 papers
and meta-analysis of 13 suitable studies quantified the excess detentions (odds ratio for being
compulsorily detained under mental health legislation if Black vs White = 4.3) [3].
2c: Quantitative surveys of socio-cultural determinants of mental health inequalities (2001-
08). Bhui et al undertook a series of surveys of discrimination / work stress and common mental
disorders, of which one secondary analysis showed that discrimination was an important risk factor
for common mental disorders [4]. Other studies implicated explanatory models and coping; and
socio-economic risk factors of common mental disorders [4]. This involved developing and
validating new survey instruments (eg the Barts Explanatory Model Interview) [5].
2d. Analysis of national suicide statistics by ethnic group (2006-07). Bhui led a national
evaluation of suicide and ethnicity [6] that documented a highly significant excess of suicide in
young (13-24 year old) black Caribbean and African men compared to white British men of the
same age. These findings were evident in both community and inpatient settings. The team also
showed that, in contrast to previous studies, South Asian women did not have significantly higher
rates of suicide. In a report to the Department of Health, the team demonstrated a near-absence of
community-based suicide prevention initiatives, and notably none aimed at high-risk Black men.
Queen Mary researchers included Professors Bhui, Stansfeld, Priebe, and Feder and Hull.
References to the research
Six papers listed of 40 relevant from this group (Queen Mary researchers in bold):
1. Bhui K, Brown P, Hardie T, Watson JP, Parrott J. African-Caribbean men remanded to Brixton
Prison. Psychiatric and forensic characteristics and outcome of final court appearance. British
Journal of Psychiatry 1998; 172: 337-44.
2. Bhui K, Bhugra D, Goldberg D, Dunn G, Desai M. Cultural influences on the prevalence of
common mental disorder, general practitioners' assessments and help-seeking among Punjabi
and English people visiting their general practitioner. Psychological Medicine 2001; 31: 815-25.
3. Bhui K, Stansfeld S, Hull S, Priebe S, Mole F, Feder G. Ethnic variations in pathways to and
use of specialist mental health services in the UK. Systematic review. British Journal of
Psychiatry 2003; 182: 105-16.
4. Bhui K, Stansfeld S, McKenzie K, Karlsen S, Nazroo J, Weich S. Racial/ethnic discrimination
and common mental disorders among workers: findings from the EMPIRIC Study of Ethnic
Minority Groups in the United Kingdom. American Journal of Public Health. 2005; 95: 496-501.
5. Bhui K, Rüdell K, Priebe S. Assessing explanatory models for common mental disorders.
Journal of Clinical Psychiatry 2006 67: 964-71.
6. Bhui K, McKenzie K. Rates and risk factors by ethnic group for suicides within a year of
contact with mental health services in England and Wales. Psychiatric Services 2008;59:414-6.
Details of the impact
4a. Informing public and professional debate on a sensitive issue
The findings emerged in the context of some high-profile deaths of Black men in UK psychiatric
hospitals, and raised awareness of ethnic inequalities in mental health. Prior to this research, the
prevailing paradigm for explaining these inequalities was `racism'. Not only was this an inaccurate
interpretation of the evidence; it also diverted policy attention into simplistic solutions (eg tick-lists
of `cultural competencies' in which staff would need to be trained), and to undermine efforts of NHS
organisations and staff to provide effective and personalized care taking account of culture.
Research in Queen Mary has steadily shifted this paradigm towards more nuanced and socio-
culturally informed perspectives. For example, the excess of compulsory detentions of Black men
for psychosis may be due in small part to `racism' or `cultural stereotyping', but a full explanation
must include other interacting variables, including poverty; educational background; stress and
discrimination in the workplace; cross-cultural differences in expressions of distress; differences in
family support and help-seeking behaviour; and medication adherence. The findings of this
research and evaluation of the national programme [7] led to the recognition among policymakers
that solutions must go beyond a behaviourist emphasis on `racial awareness' to embrace
organisational and systemic changes as well as personal culture and poor cultures of care.
4b. Informing and developing national legislation and policy (includes):
- Revisions to the Mental Health Bill 2006. This research was reviewed and evidence taken
when the new bill was being developed. The findings, cited in the consultation documents [8],
helped halt legislation that was feared to risk greater ethnic inequalities in use of the Mental
Health Act. The final Bill was modified in a way that was unlikely to further increase inequalities
in detention, and further research is investigating what explains increasing levels of compulsory
detention in hospital in all groups, and the persistent excess among black patients.
- Prof Bhui was invited to draft national policy in 1999-2004; this work produced a 5 year plan
(`Delivering Race Equality 2005-2010' [9]) incorporating new service models, training and
further research. Many impacts resulted from this policy in 2008-13. In many localities,
communities had a greater say in local services and were more engaged with NHS services by
informing the implementation of the Race Relations Amendment Act and by promoting more
sophisticated models of workforce development to meet the needs of culturally diverse
populations. Most importantly, every trust was charged with improving their delivery of care to
minority ethnic groups and to show this in inspections to the Regulator. Other impacts include:
- Prof Bhui co-authored a report to the Department of Health on suicides in Black and Minority
Ethnic (BME) groups [10], contributing to the emphasis in the newly launched (Sept 2012)
National Suicide Prevention Strategy and to the work of the 2006 strategy as part of the
`Delivering Race Equality' programme.
- A national Race Equality & Cultural Competence programme (RECC) was mandated for all
mental health professionals, driven by strategic health authorities (SHAs) [11]. It led to
inclusion of training by the Care Quality Commission in a race impact assessments of SHAs.
-
Five hundred `race equality leads', a new workforce, were introduced nationally requiring
each Strategic Health Authority to develop an action plan [12].
- As part of developing a competent and informed workforce to reduce inequalities, with pump-
priming funds from Department of Health, Bhui set up an MSc in 2002 (plus Certificate and
Diploma) in Transcultural Mental Health, delivered in an innovative online format to 80
students annually, now drawn from over 38 countries. This course has recently been extended
with new pathways in Psychological Therapies, and Mental Health & Law [13].
4c. Informing and developing national and international guidelines
This work has been cited by, and strongly influenced, guidelines by the National Institute of Health
and Clinical Excellence on schizophrenia, for which Bhui chaired the access and engagement
panel [14]; the World Psychiatric Association Guidelines on Mental Health of Migrants [15];
European Union Guidelines on Healthcare of migrants: EU-COST action [16]; and European
Psychiatric Association guidelines on Public Mental Health [17].
4d: Implementing and evaluating new care pathways in the NHS
The action research project led by Queen Mary (2005-2007) `Enhancing Pathways Into Care'
(EPIC) in four NHS trusts illustrated a range of ways of changing pathways into care and engaging
hard-to-reach groups to improve access, often through partnerships between voluntary and
statutory sector agencies [18]. For example, a Pakistani Muslim Centre developed a joint
assessment protocol with an early intervention team in order to improve access to psychiatric care
for women from this otherwise isolated population. In one site (Sheffield) local audits showed a
small reduction in the average duration of admissions among Black people. The evaluation showed
clinical leadership, transformational leadership and cultural confidence were key ingredients to the
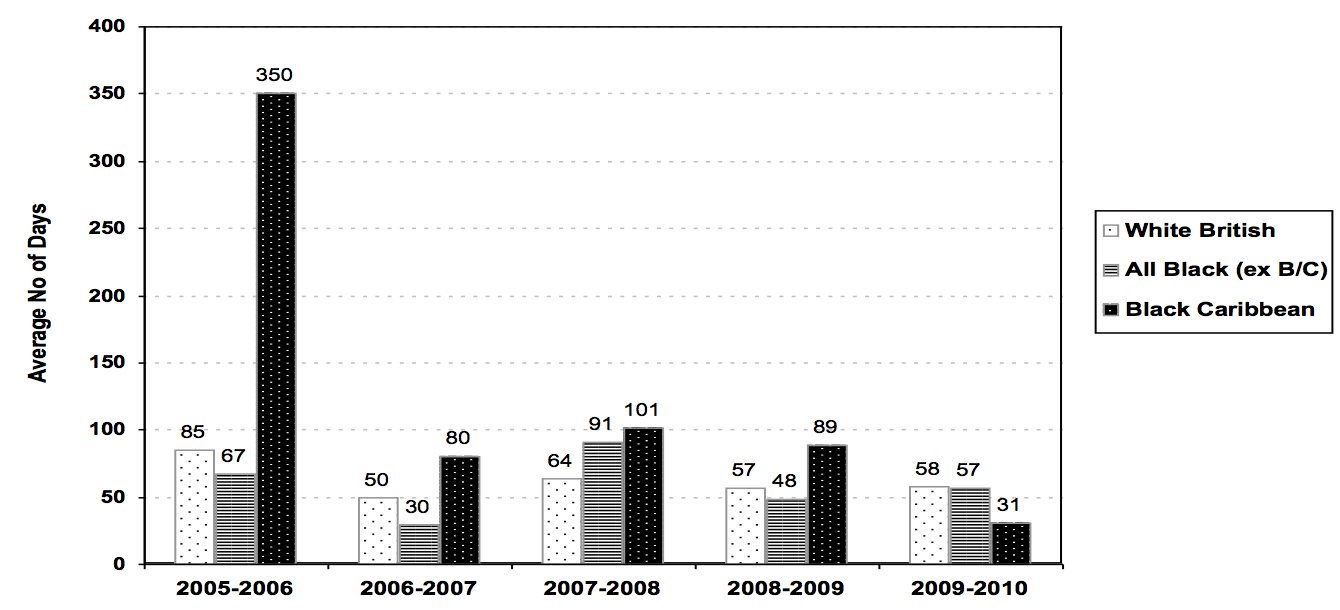
genuine change in services. The graph below (from a peer-reviewed publication in Transcultural
Psychiatry) shows one example of reduction in average length of stay in Black patients on
admissions on wards in Sheffield in a participating unit in the EPIC project in 2005-7.
4e: Informing and influencing training and workforce development
The Queen Mary team were commissioned by NHS Tower Hamlets (£450K) to provide the
Cultural Consultation Service to address intersectional inequalities arising in clinical practice.
Bhui set this up to provide individual staff training in holistic, socio-culturally informed care as well
as organisational and system-level support and guidance to NHS organisations seeking to reduce
inequalities in mental health service provision [19]. This is built on anthropological understandings
of culture, which notes the significance of beliefs, arts, laws, morals and behaviours found in all
ethnic groups. The model uses patient and staff narratives of care as the basis for intervention
alongside ethnographic research methods for evaluation. The team imported and adapted a
Canadian model to provide a new service, including in-service workforce development by teaching
staff how to use a cultural formulation, and addressing commissioning, management and team
influences. This and the narrative approach permitted more negotiated care plans for patients who
were disengaging or stuck in assertive outreach or other specialist psychiatric teams. The service
also included organizational analyses to assist the services and teams to adapt their ways of
working to reduce inequalities. Bhui led an audit of this service showing over 900 contacts, and
that cultural competency of staff improved [20]. Among a small sample of complex patients (n=36)
needing specialist and in-depth work, there were significant cost savings (£18K total) at three
month follow up. Patient functioning improved and trends showed fewer unmet needs.
4f: Informing further research
The overall picture nationally from the Care Quality Commission is that despite an evidence-based
intervention based on this research, there has been no overall reduction in ethnic inequalities in
detentions, ie that dramatic improvements in some areas (see graph above) are counterbalanced
by worsening inequalities in other areas. This has prompted new collaborative NIHR-funded
research studies to explore variations in compulsory admissions across the country [21].
Hypotheses include various geographical factors and social determinants of health.
4g: Oral and written evidence to Home Office and Government: Bhui's team undertook
research on Khat (widely used in some minority ethnic groups and linked to mental health
problems) and presented the case for it being made illegal [22].
Sources to corroborate the impact
- National Institute of Mental Health England 2003: `Inside Outside: Improving Mental Health
Services for BME Communities in England' (includes 27 references to Queen Mary research)
Inside Outside: Improving mental health services for BME communities in England.
- Mental Health Bill 2006. Hansard record of Queen Mary research being discussed in House of
Lords debate on this Bill: www.theyworkforyou.com/lords/?id=2006-11-
28c.679.2&s=Bhui#g704.0
- Department of Health and National Mental Health Development Unit. `Delivering Race Equality
in Mental Health Care: A Review' 2009 (www.nmhdu.org.uk/silo/files/delivering-race-equality-
in-mental-health-care-a-review.pdf, see page 11) includes EPIC evaluation lead by Bhui:
www.wolfson.qmul.ac.uk/psychiatry/epic
- National Mental Health Development Unit: `Suicide Prevention for BME Groups in England'
2006: www.nmhdu.org.uk/silo/files/suicide-prevention-for-bme-groups-in-england.pdf
- Race Equality and Cultural Competence programme (RECC), see `Delivering Race Equality in
Mental Health Care: A Review' 2009: www.nmhdu.org.uk/silo/files/delivering-race-equality-in-
mental-health-care-a-review.pdf
- Ministerial statement announcing 500 community development workers as race equality leads:
www.publications.parliament.uk/pa/cm200405/cmhansrd/vo050111/wmstext/50111m01.htm
- Training courses: www.wolfson.qmul.ac.uk/psychiatry/courses/ and
www.qmul.ac.uk/events/items/2012/83195.html
- NICE Guideline on Schizophrenia (updated 2010) www.nice.org.uk/CG82 See pages 9,10,11
and 30. Bhui et al, 2007 cited here has been accessed 28,648 times.
- World Psychiatric Association guidance on caring for migrants with mental health needs.
Bhugra, Gupta, Bhui et al, World Psychiatry 2011 10: 2-10.
www.wpanet.org/detail.php?section_id=7&content_id=895
- European Union Guidelines on Healthcare of migrants: EU-COST action:
www.cost.eu/domains_actions/isch/Actions/IS0603?management
- Campion J, Bhui K, Bhugra D. European Psychiatric Association (EPA) guidance on
prevention of mental disorders. European Psychiatry 2012; 27: 68-80.
- Reports on EPIC project. All papers listed here:
www.wolfson.qmul.ac.uk/psychiatry/epic/epicppublications.html, published in: International
Review of Psychiatry 2009; 21: 425-6, 450-9, 460-4, 465-471, 482-5. By Bhui, Moffatt,
McKenzie, Sass: www.wolfson.qmul.ac.uk/psychiatry/epic/epicevaluation.html
- Cultural Consultation website www.culturalconsultation.org
- Audit of Cultural Consultation Service. http://www.culturalconsultation.org.uk/wp-
content/uploads/2013/10/CCS-Final-report.pdf [available in archive]
- www.netscc.ac.uk/hsdr/projdetails.php?ref=10-1011-70
- Advisory Committee on Drug Misuse: Khat: A review of its potential harms to the individual and
communities in the UK. www.homeoffice.gov.uk/publications/agencies-public-
bodies/acmd1/ACMD-khat-report-2013/report-2013?view=Binary