Improved sensitivity of breast cancer screening with two-view mammography
Submitting Institution
Queen Mary, University of LondonUnit of Assessment
Clinical MedicineSummary Impact Type
HealthResearch Subject Area(s)
Medical and Health Sciences: Oncology and Carcinogenesis, Public Health and Health Services
Summary of the impact
As a result of research at Queen Mary, an estimated 2,500-3,000
additional women per year in UK have a breast cancer detected early
through two-view mammography at the NHS Breast Screening Programme, and
similar country-wide benefits have occurred abroad. From 1988 the NHS
Breast Screening Programme offered women aged 50-64 three-yearly one-view
mammography. In 1995, results from the UKCCCR Randomised Trial of One and
Two View Mammography (led by Queen Mary researchers) showed that including
a second view increased breast cancer detection by 24% and reduced recall
rate by 15%. On the basis of this evidence, the Department of Health
immediately issued an Executive Letter requiring all breast screening
units to move to two-view mammography for the prevalent screen. Changes
were rapidly and widely implemented. By 2004, two-view mammography had
become the policy at all screens, prevalent and incident. Two-view
mammography remains national policy and its benefits continue to the
present day.
Underpinning research
Breast cancer is by far the commonest female cancer in the UK, accounting
for 31% of all new cases of cancer in women; 50,000 new cases are detected
annually. Mammography detects most (though not all) breast cancers before
they are clinically apparent, allowing treatment to commence earlier and
extending long-term survival. Since 1988, the National Breast Cancer
Screening Programme has offered three-yearly mammography to women aged
50-64 (more recently, those aged 50-70). Over 2 million such women are
screened in the UK annually.
The original National Breast Screening Programme was based on Swedish
research that had used one-view mammography. In the early 1990s, the
sensitivity, specificity and cost-effectiveness of one- versus two-view
mammography was unknown and there was concern to optimise these metrics.
Researchers at the Wolfson Institute for Preventive Medicine at Queen
Mary, led by Professor Nick Wald, were commissioned by the UK Coordinating
Committee on Cancer Research (UKCCCR) to undertake a trial comparing these
options in the prevalent round of breast screening.
The UKCCCR Randomised Controlled Trial of One- and Two-View Mammography,
which finished recruiting in 1994, was designed to compare one-view
mammography (medio-lateral oblique, MLO in Figure 1) and two view
(medio-lateral oblique, and cranio-caudal, CC in Figure 1) in breast
cancer screening [1]. From nine breast screening centres in England,
40,163 women aged 50-64 attending their first breast screening examination
were randomised to have one-view, two-view or two-view mammography in
which one view was read by one reader and both views were read by another.
Readers were blinded to whether a second view existed (to exclude a
possible bias due to the reader knowing that a second view was available
if they needed it).
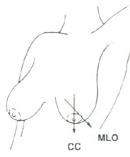 Figure 1: Two different views of the breast taken in mammographic screening: medio-lateral oblique (MLO) and cranio-caudal (CC)
Figure 1: Two different views of the breast taken in mammographic screening: medio-lateral oblique (MLO) and cranio-caudal (CC)
The results, published in 1995, showed that two-view mammography detected
24% more women with breast cancer (95% CI 16% to 31%) than one-view [1].
Prevalence of detected cancer was 6.84 per 1,000 women with two-view and
5.52 with one-view mammography. The proportion of women recalled for
assessment was 15% lower (95% CI 6% to 23%) with two-view (6.97%) than
with one view (8.16%) mammography. The cost of two-view screening was
higher (£26.46 compared with £22 per examination, 1995 prices) but the
average cost per cancer detected was similar (£5,330 compared with £5,310)
and the marginal cost per extra cancer detected with two views was similar
to the average cost (£5,400).
In sum, the study demonstrated conclusively that two-view mammography was
medically more effective than one-view; it detected significantly more
cancers and reduced recall rates; and it was also similarly cost effective
even when only considering short-term costs (ie without taking account of
the additional cost savings to the NHS of fewer recalls and fewer
late-detected cancers).
In a subsequent study to explore the radiographic reasons why two-view
mammography was superior to one-view, mammograms from 110 women whose
breast cancer had been detected in the screening programme were retrieved
from the screening centres and shown to three consultant radiologists
(working independently) [2]. Of the 110 women, 87 had their breast cancer
detected by both one and two views and in 23 it was missed by one view but
detected using two views. Outcome measures were breast size, location and
size of the cancer, mammographic features, presence of micro-calcification
and overall radiological assessment. Although 23 cancers were missed in
the original trial when one view was used, only two were not visible on
the oblique view. Cancers missed using a single oblique view (and only
detected if the cranio-caudal view was available with the oblique) tended
to be smaller by about 4 mm (P = 0.05), centrally located in the breast (P
= 0.16), not spiculated or round, (P ≤ 0.001) and lacked
micro-calcification (P = 0.15). Other variables were non-significant. The
authors concluded that the basis of two-view mammography was the added
value of the second view for detecting cancers with these features.
More recently, a study led by Queen Mary researchers confirmed that the
cranio-caudal view in two-view mammography provides critical information
for breast density estimation [3].
References to the research
1. Wald NJ, Murphy P, Major P, Parkes C,
Townsend J, Frost C. UKCCCR multicentre randomised controlled
trial of one and two view mammography in breast cancer screening. BMJ:
British Medical Journal 1995; 311: 1189-93.
2. Hackshaw AK, Wald NJ, Michell MJ, Field S, Wilson ARM.
An investigation into why two-view mammography is better than one-view in
breast cancer screening. Clinical Radiology 2000; 55: 454-58.
3. Duffy SW, Nagtegaal ID, Astley SM, Gillan MG, McGee MA, Boggis
CR, Wilson M, Beetles UM, Griffiths MA, Jain AK, Johnson J, Roberts R,
Deans H, Duncan KA, Iyengar G, Griffiths PM, Warwick J, Cuzick J,
Gilbert FJ. Visually assessed breast density, breast cancer risk and the
importance of the craniocaudal view. Breast Cancer Res 2008; 10:
R64
Details of the impact
4a. Change in UK breast screening policy
The Department of Health (which was aware of the findings of the trial
some months before the BMJ publication appeared) issued an Executive
Letter in early 1995 requiring all breast screening units to move, within
8 months, to two-view mammography for the prevalent screen [4]. There was
some uncertainty about whether the full benefit of two views could be
realised in practice, especially since the NHS Breast Screening Programme
was under workload pressures. For this reason, the introduction of
two-view mammography was initially restricted to the prevalent (ie first
screening) round while one view was used for incident (ie subsequent
screening) rounds [5].
In September 2000, the Department of Health published The Cancer
Plan, which announced the intention to introduce two views into
every attendance at the NHS Breast Screening Programme by December 2003
[6].
4b. Change in clinical practice
Many UK breast screening units adopted the two-view approach back in
1995-96 in accordance with the research findings and Executive Letter [4],
and the rest followed. By December 2003, 90% of the programmes had
achieved the target set out in The Cancer Plan, with the remaining
10% projected to do so shortly afterwards [6]. Two-view mammography is now
routine in the UK setting.
4c. Improved sensitivity and specificity of cancer detection
Between 1997 and 2005, the NHS Breast Screening Programme undertook a
series of audits of the impact of one- and two-view screening protocols.
One audit, for example, compared the cancer detection rates in the
incident round of those programmes that had introduced two views at every
attendance with the majority of programmes that used single view for the
incident round [7]. They found the two-view programmes detected 42% more
small invasive cancers (<15mm) — a rate at least as good as, and
perhaps even better than, the results obtained from the randomised trial —
and also that two views helped to protect against observer error (in which
some but not all assessors would be able to detect a small cancer on a
single view but far more would detect it on two views). The reduction in
recall rate predicted by the trial took some years to establish and may be
partly attributable to other influences (eg more double reading of films).
An audit of the NHS Breast Screening Programme in 2000-05 showed a 20%
increase in overall incident screen cancer detection rate, with the
biggest effect seen for small (<15 mm) invasive cancers [8,9]. This
increased detection rate was achieved with an 11% drop in recall rate.
Similarly, an audit of the Welsh National Breast Screening Programme
between 2000 and 2005 [10] compared 98,752 women who had single-view
mammography with 95,464 who had two-view. Five hundred and fifty-five
cancers were detected with one view and 744 with two, an increased
detection rate from 5.6 to 7.8 cancers per 1000 women screened — a 39%
increase (p=0.01) [10]. Two hundred and thirty-nine small (ie early,
potentially curable) cancers were detected with one view and 323 with two,
increasing the detection rate of these cancers from 2.4 to 3.4 per 1000
women screened — a 42% increase (p=0.05).
In 2004, the Director of the NHS Cancer Screening Programme summed up the
benefits of this change in screening practice in the Journal of Medical
Screening:
"The move from single view at every round to two views at every round
has been an evidence-based, cost-effective quality improvement. It has
contributed to the high-quality NHS BSP [Breast Screening Programme]
operating currently." (page 56) [5].
4e. Quantified estimates of benefits continuing during the impact
period 2008-13
In 2008, a review of advances in breast cancer screening named the
introduction of two-view mammography as one of the three most significant
advances in breast cancer screening in the previous 20 years [11]. These
early improvements in sensitivity and specificity are now beginning to
have long-term impacts on morbidity and mortality (because a small breast
cancer detected through screening would typically have taken many years to
kill the patient had it gone undetected). Thus, whilst the improvements in
sensitivity and specificity of national breast screening programmes began
before 2008, it has continued and (because of progressively increased
uptake around the world) extended further year on year.
Two-view mammography remains the national gold standard and this is a
direct result of the UKCCCR trial results published in 1995. It continues
to have significant health impacts up to the present day, since the same
policy and practice remains in place.
An audit undertaken by Queen Mary researchers in 2010-12, based on the
national cohort of women who were first screened with either one-view or
two-view mammography in 2003-04 and/or in 2004-05 and who were then
followed up for up to three years, showed that there was a highly
significant reduction in subsequent interval cancers: the incidence of
such cancers with two-view mammography was 0.68 relative to the incidence
with one-view mammography [12].
To illustrate the sustained quantitative benefits of this research, we
cite figures from 2010-11 [13]. The NHS Breast Screening Programme
screened 2,221,938 women in England, Wales, Northern Ireland and Scotland
between April 2010 and March 2011. 17,838 cancers were detected in women
of all ages; 80% were invasive. Cancer detection rates for all cancers
were 8.0 per 1,000 women screened and for small invasive cancers (<15mm
in diameter — the ones that are typically too small to be felt) were 3.3
per 1,000 women screened. Using the (relatively conservative) figure of
39% for the incremental detection rate with two-view mammography, it is
estimated that around 2,500-3,000 invasive cancers are now detected in UK
annually (many of them early and treatable) that would have been missed if
one-view mammography remained the norm [13].
4e. Impact on screening programmes and cancer detection beyond UK
The use of two-view mammography in breast screening is now recommended by
numerous professional bodies worldwide, including the World Health
Organisation's 2006 recommendation, which is still current [14]. The US
National Cancer Institute acknowledges the superiority of two-over
one-view mammography [15].
Two-view mammography is now practised in almost all screening programmes.
In EUNICE, a systematic data warehouse on breast cancer screening in
Europe, a review in 2012 of 25 national and regional programmes in Europe
found that all used two-view mammography at prevalent screen and 64% (16
out of 25) used two-view at all screens [16].
Sources to corroborate the impact
- Winyard G. Executive Letter (95) 7. Quality in the NHS Breast
Screening Programme. London: Department of Health, 1995.
- Patnick J. NHS breast screening: the progression from one to two
views. Journal of Medical Screening 2004; 11: 55-56.
- Department of Health. The Cancer Plan: A Plan for Investment, A
Plan for Reform. London, 2000.
- Blanks RG, Moss SM, Wallis MG. Use of two-view mammography compared
with one view in the detection of small invasive cancers: further
results from the National Health Service breast screening programme. Journal
of Medical Screening 1997;4: 98-101.
- Blanks R, Bennett R, Patnick J, et al. The effect of changing from one
to two views at incident (subsequent) screens in the NHS breast
screening programme in England: impact on cancer detection and recall
rates. Clinical Radiology 2005; 60: 674-80.
- Bennett R, Blanks R, Patnick J, et al. Results from the UK NHS breast
screening programme 2000-05. Journal of Medical Screening 2007;
14: 200-204.
- Osborn G, Beer H, Wade R, et al. Two-view mammography at the incident
round has improved the rate of screen-detected breast cancer in Wales. Clinical
Radiology 2006; 61: 478-82.
- Hogben RK. Screening for breast cancer in England: a review. Current
Opinion in Obstetrics & Gynecology 2008; 20: 545-9.
- Dibden J, Offman J, Parmar D [et al...], Duffy S. Reduction in
interval cancer rates following the introduction of two-view mammography
in the UK breast screening programme. British Journal of Cancer
2013, in press.
-
NHS Breast
Screening Programme Statistical Bulletin (England) 2011 - 2012
(www.hscic.gov.uk/catalogue/PUB10339).
- Guidelines for the early detection and screening of breast cancer.
World Health Organization, Regional Office for the Eastern
Mediterranean, 2006. (see page 36).
- US National Cancer Institute `PDQ': Breast Cancer Screening —
Mammography online guidance. www.cancer.gov/cancertopics/pdq/screening/breast/healthprofessional/page5
- Giordano L, von Karsa L, Tomatis M, et al. Mammographic screening
programmes in Europe: organisation, coverage and participation. Journal
of Medical Screening 2012; 19 (S1): 72-82.