The evidence base for harms from environmental tobacco smoke
Submitting Institution
Queen Mary, University of LondonUnit of Assessment
Clinical MedicineSummary Impact Type
HealthResearch Subject Area(s)
Medical and Health Sciences: Public Health and Health Services
Summary of the impact
Epidemiological research at Queen Mary, commissioned by the Department of
Health, demonstrated a clear and causal link between exposure to
environmental tobacco smoke and both ischaemic heart disease and lung
cancer. The evidence contributed significantly to public and political
debates on whether to ban smoking in public places. It informed the
rebuttal of heavy tobacco industry lobbying and had a pivotal influence on
changes in the law in Scotland (2006), England and Wales (2007), and
Northern Ireland (2007), as well as in many countries outside UK, which
led to highly significant reductions in environmental pollution from
secondhand smoke. Many health benefits were subsequently attributed to the
ban, notably a 17% reduction in incidence of acute myocardial infarction.
Underpinning research
The Wolfson Institute of Preventive Medicine at Queen Mary has a long
tradition of undertaking policy-relevant research (empirical studies and
systematic reviews and meta-analyses) to identify environmental harms with
a view to informing changes in policy and legislation. Here, we describe
the most significant programme of work since 1993, which built the
evidence base on passive smoking and informed the far-reaching legislative
changes banning smoking in public places.
In 1996, the Department of Health (DH) (England) commissioned Professor
Wald's team to prepare a report to evaluate the strength of evidence on
the harmful effects of environmental tobacco smoke and quantify the risk.
A background paper [1] and two shorter BMJ publications resulted [2,3].
Particularly innovative was the paper on ischaemic heart disease [2]. In
this meta-analysis, Wolfson researchers included all 19 acceptable
published studies of heart disease risk in lifelong non-smokers who lived
with a smoker and in those who lived with a non-smoker, five large
prospective studies of smoking and ischaemic heart disease, studies of
platelet aggregation and studies of diet according to exposure to tobacco
smoke. The relative risk of ischaemic heart disease with exposure to
environmental tobacco smoke was 1.30 (95% CI 1.22 to 1.38) at age 65. At
the same age, the estimated relative risk associated with smoking one
cigarette per day was similar at 1.39 (1.18 to 1.64), while for 20 per day
it was 1.78 (1.31 to 2.44).
The researchers were the first to recognise that this result from several
large rigorous cohort studies established that the dose-response
relationship between tobacco smoke intake and risk of ischaemic heart
disease was non-linear, indicating that the seemingly disproportionately
large effect of passive smoking was not surprising. Two separate analyses
indicated that non-smokers who live with smokers eat a diet that places
them at a 6% higher risk of ischaemic heart disease, so the direct effect
of environmental tobacco smoke was to increase risk by 23% (14% to 33%).
Platelet aggregation provided a plausible and quantitatively consistent
mechanism for this low dose effect. The increase in platelet aggregation
produced experimentally by exposure to environmental tobacco smoke would
be expected to have acute effects that increased the risk of ischaemic
heart disease by 34%.
Whilst many primary studies already existed, fewer than half had produced
a definitive result and there was controversy about the significance of
`positive' studies, especially in relation to whether and how confounding
variables such as diet had been accounted for. In contrast, the findings
from the Queen Mary meta-analysis were definitive and compelling (Figure
1): breathing other people's smoke is an important cause of ischaemic
heart disease, increasing a non-smoker's risk by almost a quarter. The
potential impact on exposed individuals of avoiding environmental tobacco
smoke was equivalent in magnitude to someone with hypertension taking a
blood pressure-lowering drug.
The meta-analysis on environmental tobacco smoke and lung cancer [3]
followed a similar design, synthesising findings from 37 published studies
in lifelong non-smokers who lived with a current smoker or lifelong
non-smoker. The risk estimate was compared with that from linear
extrapolation of the risk in smokers using seven studies of biochemical
markers of tobacco smoke intake. Results were similar: the excess risk of
lung cancer was 24% (95% CI 13% to 36%) in non-smokers who lived with a
smoker (P < 0.001). Adjustment for the effects of bias (positive and
negative) and dietary confounding had little overall effect; the adjusted
excess risk was 26% (7% to 47%). Furthermore, the dose-response relation
of the risk of lung cancer with both the number of cigarettes smoked by
the spouse and the duration of exposure was significant, and
tobacco-specific carcinogens were found at significant levels in the blood
and urine of non-smokers exposed to environmental tobacco smoke. Again,
the conclusion was definitive and compelling: breathing other people's
cigarette smoke is a significant and preventable cause of lung cancer.
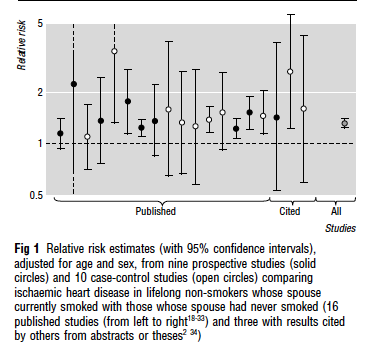 Figure 1 (reproduced from reference 2 below), showing how
meta-analysis by Wolfson researchers reduced uncertainty on the relation
between environmental tobacco smoke and ischaemic heart disease
Figure 1 (reproduced from reference 2 below), showing how
meta-analysis by Wolfson researchers reduced uncertainty on the relation
between environmental tobacco smoke and ischaemic heart disease
Further research referenced below includes a detailed exposition of the
statistical methodology used for these analyses [4] and later work in
collaboration with other research teams worldwide to update the evidence
base, partly in response to lobbying from the tobacco industry, who
initially strongly rejected the findings of the early meta-analyses
[5,6,7].
References to the research
1. Law MR, Hackshaw AK. Environmental tobacco smoke. British
Medical Bulletin 1996; 52: 22-34.
2. Law MR, Morris J, Wald NJ. Environmental tobacco smoke
exposure and ischaemic heart disease: an evaluation of the evidence. BMJ
1997; 315: 973-80.
3. Hackshaw AK, Law MR, Wald NJ. The accumulated evidence on lung
cancer and environmental tobacco smoke. BMJ 1997; 315: 980-88.
4. Hackshaw A. Lung cancer and passive smoking. Statistical
Methods in Medical Research 1998; 7: 119-36.
5. Law MR, Wald NJ. Environmental tobacco smoke and
ischemic heart disease. Progress in Cardiovascular Diseases 2003;
46.1: 31-38.
6. Vineis P, Alavanja M, Buffler P, Fontham E, Franceschi S, Gao Y, Gupta
P, Hackshaw A, Matos E, Samet J. Tobacco and cancer: recent
epidemiological evidence. Journal of the National Cancer Institute
2004; 96: 99-106.
7. Nebot M, López MJ, Gorini G, Neuberger M, Axelsson S, Pilali M,
Fonseca C, Abdennbi K, Hackshaw A, Moshammer H. Environmental
tobacco smoke exposure in public places of European cities. Tobacco
control 2005; 14: 60-63.
Details of the impact
4a. Change in perception of risk by policymakers and the public
The Department of Health, having commissioned the work, promptly accepted
the Queen Mary team's conclusions on the risk and the size of the effect.
Legislation banning smoking in public places was advocated in 1998 by the
government's Scientific Committee on Tobacco and Health, of which
Professor Wald was a member [8]. The publication of the original
meta-analyses led to widespread media coverage. Professor Law appeared on
BBC and ITV news, and was interviewed together with a tobacco industry
representative by John Humphrys on the Today Programme.
4b. Change in policy and legislation in UK
A ban on smoking in public places was proposed by the Chief Medical
Officer Sir Liam Donaldson, in his annual public health report for 2002
[9]. A Public Health White Paper, Choosing Health, published in
2004, announced a total ban on smoking in public places [10]. Following
this, there was considerable discussion in parliament on whether the ban
on smoking in public places should be partial (eg with private clubs
exempt and taking account of a possible adverse effect on businesses and
the hospitality industry) or total, including a widely publicised threat
by Sir Liam to resign if a total ban was not upheld. Legislation, which
had already come into force in Scotland in 2006 [11], was passed in
England and Wales in 2007 [12].
4c. [Failed] attempts by the tobacco lobby to rebut the research
findings
The tobacco industry undertook a sophisticated lobbying campaign, much of
it indirectly by funding the hospitality industry, in an effort to
discredit the work of Queen Mary (and other) researchers [13]. These
efforts contributed to the delay in definitive legislation in UK until
2006-7. But ultimately, clear messages from the Department of
Health-commissioned Queen Mary meta-analyses about the serious health risk
(Figure 1) outweighed speculative (and as it turned out, unfounded)
arguments about potential loss of revenue and collapse of hospitality
businesses [14,15].
4d. Change in practice: smoking bans were effectively implemented
Contrary to predictions that this law would be widely flouted, it proved
highly effective from the outset, with (for example) an estimated 98%
compliance from businesses within six months of its introduction in
England and Wales [16]. As a direct result, levels of tobacco-related
toxic chemicals (`fine particulate matter') in ambient air of bars fell by
91%, and cotinine levels in the saliva of non-smoking bar and restaurant
workers by 76%, in the same period in England [16]. Similar findings were
documented in Scotland [17]. A Cochrane review synthesised 30 studies of
exposure to second hand smoke from across the world, 19 of which measured
this using biomarkers, and confirmed a consistent and significant
reduction following the introduction of smoking bans [18]. Importantly,
there was no evidence of compensatory increases in smoking in the home —
indeed some studies documented a decline in children's exposure to tobacco
smoke at home [19, 20].
4e. Change in policy and the law beyond the UK
Smoke-free legislation is now widespread. For example, all EU Member
States have some form of regulation aimed at limiting exposure to
second-hand smoke [21,22]; most US states have also introduced such bans,
as have some low-income countries such as Vietnam and Bhutan.
4e. Reduction in smoking-related morbidity and mortality in UK and
worldwide
Smoking bans in public places have had widespread and dramatic impacts on
human health [15]. The following examples were selected from dozens of
potentially relevant ones:
- Reduced hospital admissions for acute coronary syndrome / myocardial
infarction. We cite a BMJ study based on English data and an
international meta-analysis of 10 studies that estimates a 17% reduction
in the incidence of acute myocardial infarction as a result of smoking
bans [23,24];
- Reduced hospital admissions for childhood asthma [25]; and
- Reduced pregnancy complications (preterm delivery and small for
gestational age) [26].
4f. Changes in public attitudes to smoking
Acknowledging a background trend of declining public support for smoking
in bars, workplaces and other public places, there is evidence that even
citizens initially opposed to the bans showed a shift in attitudes over
time, with a growing perception of the personal, health and environmental
benefits of smokefree policies [27-29]. Short-term quit rates reported by
the NHS Stop Smoking Service showed a 23% increase following the
introduction of the smoking ban, though rates of sustained quitting
attributable to the ban are harder to document [15].
Sources to corroborate the impact
- Poswillo DC. Report of the Scientific Committee on Tobacco and Health.
London: The Stationery Office, 1998. (ISBN 011322124x.)
- Annual Report of the Chief Medical Officer 2002. London, Department of
Health, 2003, p. 24.
- Department of Health. Choosing Health: Making Healthier Choices
Easier. London, Stationery Office, 2004.
-
The Prohibition of Smoking in Certain Premises (Scotland)
Regulations 2006.
www.legislation.gov.uk/ssi/2006/90/pdfs/ssi_20060090_en.pdf
-
Health Act 2006. Includes Smoke-free (Premises and
Enforcement) Regulations 2006. http://www.legislation.gov.uk/ukpga/2006/28/pdfs/ukpga_20060028_en.pdf
- Dearlove JV, Bialous SA, and Glantz SA. Tobacco industry manipulation
of the hospitality industry to maintain smoking in public places.
Tobacco Control 2002; 11: 94-104.
- Drope J, Chapman S. Industry efforts at discrediting scientific
knowledge of environmental tobacco smoke: a review of internal industry
documents. Journal of Epidemiology and Community Health 2001;
55: 588-594.
- Bauld L. Impact of smokefree legislation in England: Evidence review.
University of Bath, 2011. www.gov.uk/government/uploads/system/uploads/attachment_data/file/216319/dh_124959.pdf
- Department of Health. Smokefree England — One year on. London,
Stationery Office 2008.
- Semple S, van Tongeren M, Gee I, Galea K, MacCalman L. Ayres J.
Smokefree bars 07: Changes in bar workers' and customers' exposure to
second-hand smoke, health and attitudes. Final report to the Department
of Health. University of Aberdeen, the Institute of Occupational
Medicine and Liverpool John Moores University, 2009.
- Callinan JE, Clarke A, Doherty K and Kelleher C. Legislative smoking
bans for reducing secondhand smoke exposure, smoking prevalence and
tobacco consumption. Cochrane Database of Systematic Reviews
2010; 4: CD005992. DoI: 0.1002/14651858.CD005992.pub2.
- Holliday J, Moore G and Moore L. Changes in child exposure to
secondhand smoke after implementation of smoke-free legislation in
Wales: a repeated cross-sectional study. BMC Public Health 2009;
9: 430. DoI: 10.1186/1471- 2458-9-430.
- Akhtar PC, Currie DB, Currie CE et al. Changes in child
exposure to environmental tobacco smoke (CHETS) study after
implementation of smoke-free legislation in Scotland: national cross
sectional survey. BMJ 2007; 335: 545-9.
- European Commission. Towards a Europe free from tobacco smoke: policy
options at EU level, Directorate C: public health and risk assessment.
Brussels, European Commission, 2007. http://ec.europa.eu/health/ph_determinants/life_style/Tobacco/Documents/gp_smoke_en.pdf
- EU countries that limit second-hand smoke: www.smokefreepartnership.eu/smokefreemap
- Sims M, Maxwell R, Bauld L & Gilmore A. The short-term impact of
smokefree legislation in England: a retrospective analysis on hospital
admissions for myocardial infarction. BMJ 2010; 340: c2161. doi:
10.1136/bmj.c2161.
- Meyers DG, Neuberger JS, He J. Cardiovascular effect of bans on
smoking in public places. A systematic review, meta-analysis. Journal
of American College of Cardiology 2009;54:1249-55.
- Mackay D, Haw S, Ayres JG, Fischbacher C, Pell JP. Smoke-free
legislation and hospitalizations for childhood asthma. New England
Journal of Medicine 2010;363:1139-45.
- Mackay DF, Nelson SM, Haw SJ, Pell JP. Impact of Scotland's smoke-free
legislation on pregnancy complications: retrospective cohort study. PLoS
medicine. 2012;9(3):e1001175.
- Ritchie D, Amos A, Martin C. Public places after smoke-free — a
qualitative exploration of the changes in smoking behaviour. Health
& place. 2010; 16: 461-9.
- Hargreaves K, Amos A, Highet G, Martin C, Platt S, Ritchie D and White
M. The social context of change in tobacco consumption following the
introduction of `smokefree' England legislation: a qualitative,
longitudinal study. Social Science and Medicine 2010; 71:
459-66.
- Martin C, Ritchie D and Amos A. Evaluation of the smoke-free
legislation in Scotland: qualitative community study: Final Report.
Report submitted to Health Scotland 2008. www.healthscotland.com/scotlands-health/evidence/smokefreelegislation/studydetailsqualitativecommunitystudy.aspx