Developing algorithms to optimise paired kidney donation in the UK
Submitting Institution
University of GlasgowUnit of Assessment
Computer Science and InformaticsSummary Impact Type
HealthResearch Subject Area(s)
Information and Computing Sciences: Computation Theory and Mathematics
Medical and Health Sciences: Clinical Sciences
Economics: Applied Economics
Summary of the impact
Algorithms developed by University of Glasgow researchers have helped NHS
Blood and Transplant (NHSBT) tackle the complex problem of increasing the
number of kidney transplants in the UK. For people with end-stage renal
failure, the most effective form of treatment is transplantation. Dr David
Manlove's research team have developed sophisticated algorithms which
allow the NHS to help patients who require a kidney transplant, and who
have a willing but incompatible donor, to exchange their donor with that
of another patient in a similar position, in what is known as a paired
exchange. By optimising kidney exchanges, University of Glasgow research
has increased the number of transplants from paired donation by 40%
between 2008 and 2013, when measured in comparison with the number of
transplants that would have been possible with previous pairing
techniques. Dr Manlove's work with NHSBT has translated not only into
increased quality of life for patients freed from long term dialysis but
will also afford the NHS an estimated £16 million of savings over the next
10 years.
Underpinning research
A group of two or more kidney patients swapping their willing but
incompatible donors with one another in a cyclic fashion is called a
paired kidney exchange (PKE). In early 2007, NHS Blood and Transplant
(NHSBT) set up a national matching scheme to identify optimal sets of
these exchanges from among the patient and donor data on the NHSBT
database. NHSBT developed an algorithm to search the database and identify
suitable matches from a number of weighted criteria, but this algorithm
was only capable of finding PKEs involving two donor-recipient pairs and
could only handle datasets of up to 100 potential transplants.
Dr David Manlove's interests in algorithmic research into matching
problems, and his recognition of the inefficiencies in the existing model,
as well as previous collaboration with NHS Education for Scotland on the
Scottish Foundation Allocation Scheme, led to a fruitful collaboration
with the NHSBT beginning in May 2007. Manlove (Lecturer 2000-09, Senior
Lecturer 2009-present) and Dr Péter Biró (Research Assistant, 2007-10)
developed a novel approach involving graph-matching algorithms which
enabled optimal sets of PKEs, involving up to three donor-recipient pairs,
to be identified [2; 6]. They also significantly increased the capacity of
the algorithm to deal with larger datasets of up to 3,000 potential
transplants. The simulations run by the University of Glasgow team in
early 2008, using their implemented algorithms, indicated the likely
benefit, in terms of numbers of additional transplants, of allowing PKEs
to involve up to three patients rather than two. Two- and three-way PKEs
were already established in the US, but there is a complex set of
optimality criteria that made the UK application different and
algorithmically challenging. Following this initial research, the NHSBT
took the decision in April 2008 to allow PKEs to involve up to three
patient-donor pairs. The introduction of three-way exchanges meant that
this had become an `NP hard problem', meaning that an efficient algorithm
to resolve the problem was unlikely to exist, with the main risk being
that an increase in the size of the data set might cause a `combinatorial
explosion', whereby computational times become unreasonably long.
In 2010 and 2011, an improved version [5] of the Glasgow software was
written by Dr Gregg O'Malley (Research Assistant 2008-09 and 2010-11,
Research Associate 2011-13), using an integer programming technique [1].
This also addressed some changes in the established criteria for matches.
Dr O'Malley developed an in-house version of the software for the NHSBT,
allowing them to conduct the searches themselves and speed up response
times. This software was delivered to NHSBT in June 2011. O'Malley also
developed a web application [4] enabling the NHSBT to trial potential
changes to the criteria used in the matching run, which could have an
effect on the number and quality of matches. Matching runs now occur on a
quarterly basis.
The University of Glasgow researchers completed a project in 2013 which
involved further development of the kidney exchange algorithms to address
issues of scalability to ensure that they will be able to cope with even
larger datasets going forward [3]. As awareness of the National Living
Donor Kidney Sharing Schemes (the collective term used to describe the
schemes in which donated kidneys are `shared' across the UK) continues to
grow, more patients and donors are expected to join, leading to richer
datasets involving more exchanges and in turn a greater quantity and
quality of potential transplants that can be identified by the software in
the future.
The Glasgow contribution included the original research on theoretical
algorithm design, and subsequent implementation in software, leading to
deployment by NHSBT. This work is a prime example of top quality
fundamental research in matching algorithm theory, published in
peer-reviewed references [1,2],which led to extraordinary advances in real
life problems .
References to the research
1. Paper in refereed conference proceedings: D.F. Manlove and G.
O'Malley, Paired and altruistic kidney donation in the UK: Algorithms and
experimentation, in Proceedings of SEA 2012: the 11th International
Symposium on Experimental Algorithms, Lecture Notes in Computer Science,
volume 7276, pages 271-282, Springer, 2012. (doi:10.1007/978-3-642-30850-5_24/
ISBN 978-3-642-30849-9 (Key underpinning reference.) *
2. Paper in refereed journal: P. Biró, D.F. Manlove and R. Rizzi,
Maximum weight cycle packing in directed graphs, with application to
kidney exchange programs, Discrete Mathematics, Algorithms and
Applications, 1 (4) :499-517, 2009 (doi: 10.1142/S1793830909000373)
*
3. Externally-funded research project: Optimising options and
strategies for living donor kidney transplantation for incompatible
donor-recipient pairs. Duration: 1 January 2012 - 30 June 2013. Amount:
£151k. Funder: NHS Blood and Transplant. Co-Investigator: Dr David
Manlove. Research Associate: Dr Gregg O'Malley.
4. Externally-funded research project: Kidney Paired Exchange
Data Analysis Toolkit. Duration: 1 July 2011 - 31 December 2011. Amount:
£32k. Funder: EPSRC KTA fund. Principal Investigator: Dr David Manlove.
Research Associate: Dr Gregg O'Malley.
5. Externally-funded research project: Software for the National
Matching Scheme for Paired Donation. Duration: 1 April 2010 - 30 June
2011. Amount: £108k. Funder: NHS Blood and Transplant. Principal
Investigator: Dr David Manlove. Research Assistant: Dr Gregg O'Malley. *
6. Externally-funded research project: MATCH-UP: Matching Under
PreferencesAlgorithms and Complexity. Duration: 1 June 2007 - 30 June
2010. Amount: £324k. Funder: EPSRC (grant EP/E011993/1). Co-Investigator:
Dr David Manlove. Research Assistant: Dr Péter Biró.
* best indicators of quality
Details of the impact
Kidney failure has a devastating impact on patients' lives, and long-term
survival rates after transplantation demonstrate a doubled or tripled life
expectancy compared to dialysis. The NHSBT estimates that over 37,500
people in the UK have end-stage renal failure; nearly 21,000 are on
dialysis. As of 31 March 2013 there were 6,325 patients on the transplant
list for a donor kidney; the number of kidney transplants carried out each
year is less than half that number (2984 between April 2012-April 2013 of
which 1916 were from deceased donors and 1068 from living donors [NHSBT]).
The NHSBT estimates median waiting time on the transplant list at 1168
days for an adult and 354 days for a child, and according to the National
Kidney Federation approximately 400 people each year die while awaiting a
kidney transplant.
Prior to 1 September 2006, transplants could only take place between
those with a genetic or emotional connection. However, the Human Tissue
Act 2004 and Human Tissue (Scotland) Act 2006 created the legal framework
to allow transplants between strangers, thus opening up new possibilities
for living donor transplants.
Increasing the number of potential kidney matches
Research by the University of Glasgow showed how to model a complex,
hierarchical set of criteria that form the definition of an optimal set of
kidney exchanges. The algorithm developed to identify optimal sets has
been used by NHS Blood and Transplant (NHSBT) since 2008, enabling the
number of potential matches to be radically improved and resulting in more
transplants arising from identified kidney exchanges being carried out
over the last four years (see Figure 1).
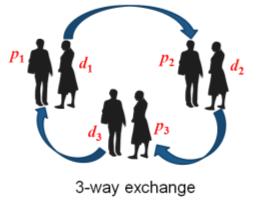
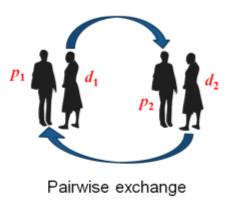 Figure 1. Shows how the kidney exchanges work: P=patient; d=donor
Figure 1. Shows how the kidney exchanges work: P=patient; d=donor
The development of the University of Glasgow algorithm led directly to a
decision by the NHS to allow three-patient `swaps' of donor kidneys from
April 2008 onwards, increasing the number of potential transplants even
further. Between July 2008 and April 2013, a total of 393 transplants were
identified by the algorithms and of these, 232 transplants actually took
place. Had the NHSBT continued to use their pre-existing algorithm, which
was only capable of identifying pairwise exchanges, it is likely that only
165 transplants would have gone ahead (from a total of 280 identified
matches, using the same conversion rate). Thus the 232 transplants that
took place represents an increase of 67, or 40%, compared to the estimated
number that would have occurred if the status quo techniques had continued
to be used.
A modified University of Glasgow algorithm has allowed altruistic donors
(people who are willing to donate a kidney to a stranger) to be included
in the National Living Donor Kidney Sharing Schemes since January 2012. An
altruistic donor can either donate directly to a patient on the Deceased
Donor Waiting List, or else trigger a domino paired donation chain
involving one or more incompatible patient-donor pairs, leading to
additional transplants.
In 2010, the Head of Organ Donation and Transplantation Studies, NHS
Blood and Transplant stated:
Since July 2008, we have been collaborating with Dr David Manlove and
Dr Péter Biró in relation to the NMSPD [National Matching Scheme for
Paired Donation, now the National Living Donor Kidney Sharing Schemes]:
their matching algorithms have been used in order to construct optimal
solutions to the datasets that we provide. Some of these datasets have
encoded particularly challenging underlying problems, and the task of
producing an optimal solution would have been highly complex without the
assistance of these matching algorithms. We anticipate that this will be
a growing issue as the number of people in the database increases over
time.
Improving patient quality of life
For patients, the benefits are numerous. Kidneys from living donors last
on average 33% longer than those from deceased donors (15 years compared
to 10), so increasing the number of these types of exchanges translates
into more patients enjoying a longer period of time living with a healthy
kidney, returning to work or otherwise resuming their normal lives.
Transplantation also extends the life expectancy of patients with kidney
disease compared to dialysis (life expectancy for dialysis patients is
only five years on average). Dialysis can save patients' lives but it is
not a cure as it does not replace all the functions of a healthy kidney.
Dialysis also carries significant health implications for patients and can
cause or contribute to anaemia, bone disease, high blood pressure, heart
disease, nerve damage and infection. A BBC
news article in March 2010 described the difference that a three-way
kidney transplant made to the lives of the recipients involved.
Financial benefits for the NHS
The work of Dr Manlove and colleagues has economic benefits for the NHS as
well as health benefits for the patients involved. According to NHSBT,
each kidney transplant saves the NHS £240,000 over 10 years (based on a
comparison with the cost of dialysis over that time period, and taking
into account the cost of the operation itself). This means that by
enabling an increase of 67 new kidney transplants, the University of
Glasgow researchers have potentially saved the NHS around £16 million over
the next 10 years, with additional savings to come with each new three-way
pairing identified.
With an aim to share best practice, compare and agree on common
optimality criteria and common data formats and lay the ground-work to
ultimately share kidney exchange pools on an international basis, Dr
Manlove and his collaborators currently have a European Cooperation in
Science and Technology proposal under review. The proposal includes
representation from the UK, France, Germany, Netherlands, Spain, Portugal,
Hungary, Czech Republic, Slovakia and wider participation from the USA and
Australia.
Sources to corroborate the impact
Evidencing value of the research to kidney donor-patient matching in the
NHS:
- Corroborating Statement from the Head of Organ Donation and
Transplantation Studies, NHS Blood and Transplant (available from HEI)
- NHSBT Paired donation website (link)
- Research Council UK, Big Ideas for the Future Report (link,
see pg 13)
- Public Service Review: Devolved Government, Vol 19 (pg36 profiles the
Glasgow research and its contribution to the NHS living donor kidney
transplant programme) [available from HEI]
- The Engineer, 18 March 2010 (link
or available from HEI)
- BBC News, 8 March 2010 (link
or available from HEI) (describes quality-of-life benefits to patients)