Improving health through an evidence-based implementation programme
Submitting Institution
University of ManchesterUnit of Assessment
Business and Management StudiesSummary Impact Type
HealthResearch Subject Area(s)
Medical and Health Sciences: Public Health and Health Services
Summary of the impact
Life for those who have had a stroke across England has been improved
through assessment of their needs six months after their stroke, followed
up with support so that these needs are met. The assessment tool used was
developed at the University of Manchester using knowledge from applied
research into knowledge translation and service improvement, which
emphasised the need for tailored, context-sensitive approaches to
implementation of evidence. The flexible assessment tool (GM-SAT) that can
be used by a range of practitioners is now in use across England in a
range of providers, enabling the fulfilment of national strategy and
improved care for these patients.
Underpinning research
The National Institute of Health Research (NIHR) Collaboration for
Leadership in Applied Health Research and Care (CLAHRC) for Greater
Manchester was established in 2008 with £20m of funding from NIHR and
local NHS partners over five years, building on a reputation for applied
health research; specifically research about knowledge translation
processes and quality improvement in health care. The CLAHRC aims to
narrow the gap between known best practice (research) and actual practice
for the care of people with cardiovascular disease.
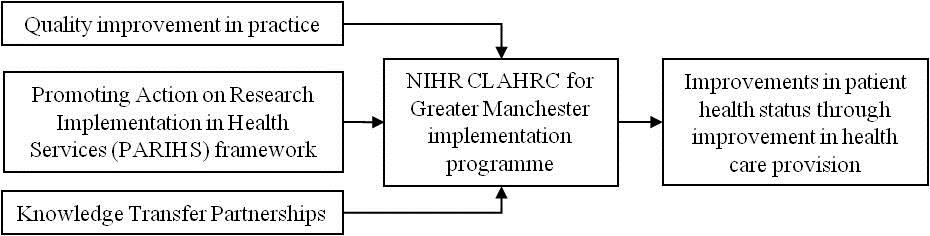
The CLAHRC approach builds on three areas of expertise within the
University of Manchester (UoM):
- Research on quality improvement in healthcare;
- Knowledge Transfer Partnership (KTP) programmes investigating the role
of facilitation in the implementation of evidence (both carried out by
Boaden and others at UMIST/UoM). Ruth Boaden has been at the University
of Manchester (and previously UMIST) since 1989 (Lecturer/SL/Professor),
and has worked with other UoM staff on various research and knowledge
transfer projects on quality improvement and healthcare since 2002.
- Harvey's previous work prior to moving to the University of Manchester
in 2003 was at the Royal College of Nursing developing a conceptual
framework to guide the implementation of evidence into practice (the
Promoting Action on Research Implementation in Health Services (PARIHS)
framework. Since that time Harvey (Senior Lecturer/Reader) has continued
work on development and testing of the PARIHS framework.
The research carried out into quality improvement in practice spans a
number of funded projects, as well as specific outputs including two books
[1,2] and included a range of KTPs. The research shows that there is most
support for models of incremental small-scale improvement; principles from
operations management underpin all approaches to improvement, and can be
applied within healthcare.
The PARIHS framework shows that successful implementation of research
evidence into practice is dependent on the complex interplay of the
evidence to be implemented (how robust it is and how it fits with
clinical, patient and local experience), the local context in which
implementation is to take place (the prevailing culture, leadership and
commitment to evaluation and learning), and the way in which the process
is facilitated (how and by whom). It was one of the earliest conceptual
models to propose this multi-dimensional view of knowledge translation in
health care and since its initial publication in 1998, it [3] has received
over 736 citations and has been used nationally and internationally as a
heuristic to guide the application of research evidence into practice and
as the conceptual underpinning of a variety of tools and frameworks to be
used at the point of care delivery, including the CLAHRC.
By combining these areas of research expertise, the CLAHRC developed a
model for the implementation of research into practice [4] embedding the
operational steps of the Model for Improvement, within the PARIHS
framework, so that the programme uses an iterative and reflective
approach to implementation. Our research also led to the inclusion
of less detail than other models about how stages of improvement should be
approached, enabling this to be determined at a local level, depending on
the local context (building again on insights from this research)
and working within multi-professional teams with designated roles
in supporting the implementation process. We have also embedded
evaluation and learning within the implementation programme to
ensure that research continues to be developed from this process.
References to the research
Quality improvement
1. Boaden R, Harvey G, Moxham C and Proudlove N (2008) Quality
Improvement: theory and practice in healthcare, NHS Institute for
Innovation and Improvement/Manchester Business School, Coventry: NHS
Institute for Innovation and Improvement, ISBN 978-1-906535-33-9 - Copy
available on request
Quality assessment: over 10,000 copies downloaded/sold
internationally, as a basis for both training and improvement
initiatives within healthcare.
2. Walshe K and Boaden R (2006) Patient safety: Research into
Practice, Open University Press - Available on request
Quality assessment: won the British Medical Association
(BMA) Book Prize for 2006 in the "Basis of medicine" category. 24 Google
scholar citations.
PARiHS framework
3. Kitson A, Rycroft-Malone J, Harvey G, McCormack B, Seers K, Titchen A
(2008) Evaluating the successful implementation of evidence into practice
using the PARIHS framework: theoretical and practical challenges. Implementation
Science, 3:1 (7 January 2008) DOI: 10.1186/1748-5908-3-1
Quality Assessment: Highly accessed paper published in
peer reviewed journal; 17,883 online accesses since publication. 283
Google scholar citations.
NIHR CLAHRC for Greater Manchester implementation programme
4. Harvey G, Fitzgerald L, Fielden S, McBride A, Waterman H, Bamford D,
Kislov R and Boaden R (2011) "The NIHR Collaboration for Leadership in
Applied Health Research and Care (CLAHRC) for Greater Manchester:
Combining empirical, theoretical and experiential evidence to design and
evaluate a large-scale implementation strategy" Implementation Science
6:1 (96) DOI:10.1186/1748-5908-6-96
Quality assessment: Paper published in peer reviewed
journal. 11 Google scholar citations.
GM-SAT post-stroke assessment tool
5. Rothwell K, Boaden R, Bamford d and Tyrrell P (2013) "Feasibility of
assessing the needs of stroke patients after six months using the GM-SAT",
Clinical Rehabilitation, 27.6 (June 2013) DOI: 10.1177/0269215512457403
http://cre.sagepub.com/content/early/2012/09/04/0269215512457403.abstract?papetoc
Quality Assessment: Paper published in peer reviewed
international journal.
Details of the impact
Context
Understanding needs and signposting to local services has been shown by
previous research to improve outcomes and quality of life for stroke
survivors, their carers and families, who want to feel supported in the
long term and have access to the medical, social and emotional support
they require as their needs change over time. A structured assessment of
people six months after discharge from hospital was one of the 20 Quality
markers in the NHS National Stroke Strategy (2007) [E] but it was not
clear what this assessment should consist of, or who should undertake it.
The CLAHRC developed and supported the implementation of a review tool to
identify needs and signpost to relevant support: the GM-SAT.
Pathway to Impact
We applied our model for implementation of research into practice to
develop the tool. Specifically we used an iterative and reflective
approach to develop the tool via workshops, consultations with
staff, patients and carers and literature reviews. As a result, the tool
has a holistic focus and is designed for use by a range of staff, not only
those with clinical qualifications. This work was carried out by a multi-professional
team with designated roles to support the process and included a
senior NHS consultant (Tyrrell), university academics (Boaden) and a
knowledge transfer associate (Rothwell). We deliberately designed the
model to be as flexible as possible, with the details determined by
facilitators at a local level, depending upon their assessment of the
local context. We also ensure that we embedded evaluation and
learning to ensure that research continues to be developed.
What is the tool?
GM-SAT is a simple, free to use, evidence-based assessment tool used to
identify and address individuals' long term, unmet post-stroke needs and
can be tailored to reflect local care pathways, services and resources
available via health and social care and the third sector. It was
developed by the CLAHRC and has subsequently been implemented across
England. GM-SAT provides everything needed to undertake a six-month
review, from the questions to ask within the review, through to
documentation for recording and communicating review outcomes to other
professionals involved in an individual's care [D]. It encompasses a wide
variety of potential post-stroke care needs from medication management and
secondary prevention through to mood and fatigue, including those required
by the Care Quality Commission's Stroke Services Review and the Department
of Health's Accelerating Stroke Improvement Programme (2010/11), as well
as the NHS National Stroke Strategy. The former National Clinical Lead for
the NHS Stroke Improvement Programme [E] has commented on the tool: "The
tool rapidly became a key element in responding to the challenge set out
in the National Stroke Strategy to take stroke seriously and start the
process of change, so that outcomes for people with stroke can be
improved. In particular, it provided an off-the-peg, validated framework
for assessing peoples' needs at 6 months after stroke, as mandated by
the Stroke Strategy."
What are the benefits of using the tool?
The benefits of using the tool are for patients and their carers, feeling
supported in the long term, and having access to the medical, social and
emotional support they require. GM-SAT has achieved significant reach
across England, being used in over a quarter of all services, because of
its acceptability to the wide range of services and professionals involved
in providing post-stroke care, who cite a number of features influencing
its uptake [A,B]:
- It is based on evidence and aligns with national clinical guidelines,
which is important for users: "GM-SAT was the best choice to meet the
requirements of National guidelines and commissioners of service".
(Stroke Occupational Therapist).
- It was developed and tested by the CLAHRC and is therefore fit for
purpose, which provides users with confidence in the tool.
- A formal evaluation has been published. We worked locally in Greater
Manchester and nationally with The
Stroke Association (SA) to pilot use of the GM-SAT by Stroke
Coordinators employed by TSA, and the evaluation of this pilot
demonstrated patient benefit [A]: Patients answered the question, `what
was good about the review?'
- "The fact that at last someone was concerned about how I was going
on after leaving hospital";
- "Being able to discuss things with someone who understands how the
stroke affects and changes a person and could help and advise on all
these points";
-
"This review has helped me to channel my thoughts as to where to go
from here, prompting some good ideas as to how to move forwards."
The long-term impact on patient outcomes would be more complex and
resource intensive to establish formally, but the inclusion of a review
in national strategy and guidance presupposes that it will benefit
patients.
- The tool is now being used through the SA to identify patients with
specific needs to participate in future research programmes,
demonstrating the research-implementation-research cycle that
characterises the CLAHRC.
- The comprehensive, tool covers health and social care needs, which
allows patients to be assessed in a holistic sense. They can then be
appropriately managed and referred on to third parties where appropriate
[B].
- Non-specialists can use the tool, and once the results are available,
this means that clinical staff have updated information available to
them, without having to conduct lengthy consultations. Unmet needs are
therefore more likely to be diagnosed and met [B].
Where and how is GM-SAT being used?
The tool was first piloted in Greater Manchester in 2009 and has
subsequently spread to a wider footprint [B] since becoming freely
available in 2010. It is used for:
- Demonstrating the need for, and then carrying out, 6-month reviews
post-stroke, as recommended by NICE guidance (Clinical Commissioning
groups (CCGs), community providers and NHS Foundation Trusts (FTs)
across London, Nottingham, and the North and East of England)
- Assessing patients with other long-term conditions
- Input to long-term community care planning where unmet needs are used
in audit to identify needs, stroke prevention issues and for feedback to
commissioners [B]
- Continuing professional development for practitioners through
development of competencies related to the domains within the tool
- Providing consistency of care across an area (Yorkshire and Humber)
through the incorporation of the tool into an IT system used by primary
and community care providers (TPP SystmOne) which means that it is tied
into the clinical record, accessible to multiple practitioners and part
of normal practice [B]
- Provision of post-stroke Information and Advice Services by the Stroke
Association, who currently provide services to over 35,000 stroke
patients through 24 services across England and have to date carried out
approximately 4000 reviews. The Chief Executive of the Stroke
Association [F] writes "As a patient advocacy organization, we are
clear that what is required 6 months post-stroke is a comprehensive
assessment which includes elements identified by stroke survivors and
their families, and GM-SAT provides this. As a result GM-SAT is the
only tool the Stroke Association offers as part of its commissioned
provision for 6 month post stroke assessments across the UK."
It has been cited as a key output from CLAHRC in the NIHR's Annual Report
for 2011 [C].
Sources to corroborate the impact
All sources cross-referenced in section 4.
[A] Evaluation of Stroke Association Pilot [http://www.stroke.org.uk/professionals/life-after/support
accessed 4 Dec 2012]
[B] GM-SAT 18 months on [http://clahrc-gm.nihr.ac.uk/ - available from 1 June 2013]
[C] NIHR Annual Report 2010/11
[D] NHS Improvement website page detailing GM-SAT tool
[E] Statement from the National Clinical Lead for the NHS Stroke
Improvement Programme (2007-2013)
[F] Statement from the Chief Executive of the Stroke Association