National Confidential Inquiry into Suicide and Homicide by People with Mental Illness
Submitting Institution
University of ManchesterUnit of Assessment
Psychology, Psychiatry and NeuroscienceSummary Impact Type
HealthResearch Subject Area(s)
Medical and Health Sciences: Clinical Sciences, Public Health and Health Services
Summary of the impact
Suicide is one of the most serious adverse outcomes in mental health
services. NCISH research is based on a comprehensive and internationally
unique database (99,000 suicide deaths; 25,000 patient suicide deaths).
NCISH impacts upon practice and policy by providing definitive figures on
suicide to clinical services and government, producing data-driven safety
recommendations and demonstrating that these recommendations reduce
suicide. Based on NCISH research, overall patient suicide rates fell by
26% (2004-11), in-patient deaths fell by 58% (2001-2010), and individual
recommendations may have prevented between 200-300 patient suicide deaths
per year. A new vehicle for impact delivery is the social enterprise Safer
Care Ltd (founded 2013), which has already reviewed 4 Trusts and, by
reinvesting future income in the social enterprise, we will continue to
meet the specific needs of mental health services.
Underpinning research
See section 3 for references 1-6; University of Manchester (UoM)
researchers are given in bold.
The impact is based on research that took place at UoM from 1996-date,
with the first major publications in 1999. The key researchers were:
-
Louis Appleby (Professor, 1996-date)
-
Jenny Shaw (Senior Lecturer, 1996-2003; Reader, 2003-2004;
Professor, 2004-date)
-
Navneet Kapur (Lecturer, 1997-2002; Senior Lecturer, 2002-2007;
Reader, 2007-2008; Professor, 2008-date)
-
Kirsten Windfuhr (Deputy Project Manager, 2002-2004; Research
Fellow/Senior Project Manager, 2004-date)
Background to the research: The aim of the research was to
recommend changes to clinical practice and policy that would reduce the
risk of suicide in mental health patients. We maintain a national register
of all suicides occurring in the UK, collecting more detailed information
directly from clinical teams on people who have been in contact with
services in the previous 12 months. Our response rates from clinicians
have been around 95% for the last 13 years. Our core database is the
largest clinical database of suicide internationally (99,000 general
population suicides; 25,000 mental health patient suicides).
Key findings: NCISH has generated key data on suicide by mental
health patients that are widely quoted:
- 1,200 people (25% of all suicides occurring in the general population)
are in contact with mental health services in the 12 months prior to
suicide (1-3);
- of this group, half are in contact with services in the week before
death (2,3).
Over the 10 year period 2001-2010:
- approximately 10% of patient suicides occur during an in-patient
admission and the commonest cause of death is by hanging (2-4); 25% of
deaths occur after patients abscond from the ward (2);
- nearly 20% of patient suicides occur within 3 months of discharge from
in-patient care; the highest risk period is the first week after
discharge, particularly the first 1 to 3 days (2,3,5);
- 14% of patients are non-adherent with drug treatment in the month
prior to suicide; 26% missed their final contact with mental health
services prior to suicide (2,3);
- receiving enhanced aftercare is a protective factor (5).
- In the Lancet 2012 paper (6) we showed that the implementation
of our recommendations was associated with a fall in patient suicide
between 1997-2006, which guided the continuity of the impact during this
assessment period. Specifically, suicide rates decreased to a greater
degree in services which implemented more of the safety measures than
those which implemented fewer. Three recommendations in particular
(24-hour crisis teams, dual diagnosis policies, multi-disciplinary
reviews following patient suicide) were associated with falls in suicide
after implementation (6). There was also evidence that recommendations
designed for particular patient sub-groups (e.g., mental health
in-patients; patients recently discharged) produced specific reductions
in suicide of between 11-32% (6).
References to the research
NCISH research has been published in top general medical and psychiatry
journals internationally. In terms of volume of outputs in the field of
suicidal behaviour over the last 5 years we are 3rd worldwide
(n=119), and 3rd worldwide in the average number of citations
per output (6.2) (Source: Scopus).
Key publications:
1. Appleby L, Shaw J, Amos T, McDonnell R, Harris C, McCann K,
Kiernan K, Davies S, Bickley H, Parsons R. Suicide within 12 months of
contact with mental health services: national clinical survey. BMJ.
1999;318(7193):1235-9. DOI: 10.1136/bmj.318.7193.1235
3. Windfuhr K, Kapur N. Suicide and mental illness: A clinical
review of 15 years findings from the UK National Confidential Inquiry into
Suicide. British Medical Bulletin. 2011;100(1):101-21. DOI:10.1093/bmb/ldr042
4. Kapur N, Hunt IM, Windfuhr K, Rodway C, Webb R, Rahman
MS, Shaw J, Appleby L. Psychiatric in-patient care and suicide in
England, 1997 to 2008: A longitudinal study. Psychological Medicine.
2013;43(1):61-71. DOI:10.1017/S0033291712000864
5. Bickley H, Hunt IM, Windfuhr K, Shaw J, Appleby L, Kapur N.
Suicide within two weeks of discharge from psychiatric inpatient care: A
case-control study. Psychiatric Services. 2013;64(7):653-9. DOI:10.1176/appi.ps.201200026
6. While D, Bickley H, Roscoe A, Windfuhr K, Rahman S, Shaw
J, Appleby L, Kapur N. Implementation of mental health service
recommendations in England and Wales and suicide rates, 1997-2006: A
cross-sectional and before-and-after observational study. The Lancet.
2012;379(9820):1005-12. DOI: 10.1016/S0140-6736(11)61712-1
Details of the impact
See section 5 for corroborating sources S1-S9.
Context
- Since the inception of NCISH in 1997, reporting of suicides by mental
health patients has increased from 20% to 95% of cases.
- NCISH is internationally unique in mental health care in terms of the
depth and breadth of information that we can provide to inform clinical
practice and suicide prevention policy (locally, nationally,
internationally).
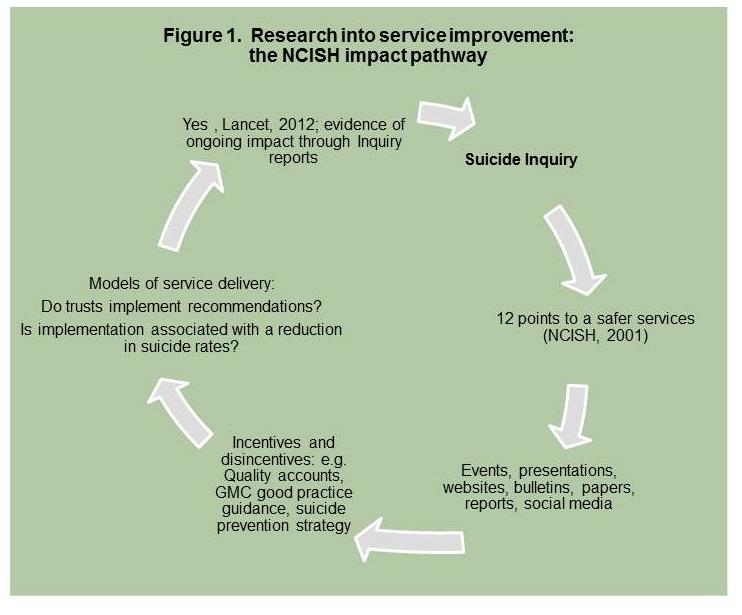
Pathways to impact (see also figure 1 below)
NCISH has provided, and continues to provide, new information to health
services and the wider community on suicide in mental health patients.
Based on this information, NCISH has made specific recommendations for
preventing suicide in services in our reports, "12 points to a Safer
Service" (S1) two iterations of the national suicide prevention strategy
for England (2002 and 2012) (S2) and international policy documents (S3,
S4). Unique to mental health services, implementation of NCISH
recommendations to clinical practice and policy has led to a reduction in
suicide rates that is ongoing and sustainable. As of 2013, additional
delivery of NICSH impact on practice and policy is carried out via the
social enterprise Safer Care Ltd.
Reach and significance of the impact
Impact on policy nationally and internationally
A major impact of NCISH research has been to inform policy through
national policy documents and answers to parliamentary questions (S5). Our
research underpins section 1 of the national suicide prevention strategy
for England (2012), Preventing suicide in England: A cross- government
outcomes strategy to save lives, which has reduced suicide in high
risk groups (S2). Section 1.13 makes specific reference to NCISH
recommendations as providing key guidance for mental health services; 2
NCISH publications are also referenced in the Strategy. Internationally,
our work has informed surveillance schemes in Ireland (e.g., the National
Suicide Research Foundation (NSRF)) and Norway (S3, S4). Our research has
also led recently to national tools for quality improvement. Our safer
mental health services toolkit (launched January 2013) has been downloaded
approximately 1,300 times to date (S6). A further example of recent impact
is the requirement for NHS Trusts to demonstrate their adherence to
Inquiry recommendations — the first Quality Accounts began in 2010/11
(S7).
Impact on services
- NCISH's focus on in-patient safety has been associated with a halving
in the number of in- patient suicide deaths. We demonstrated that three
of the NCISH recommendations were significantly associated with a
reduction in suicide rates in the NHS Trusts that had implemented them,
with no significant reduction in suicide rates in Trusts that did not
implement recommendations. Implementation of 24-hour crisis teams, dual
diagnosis policies and multi-disciplinary reviews following a patient
suicide were associated with 200-300 fewer patient deaths per year. The
cost of each suicide death is around £1.5 million (Journal of Crisis
Intervention & Suicide (2007) 28:89-94). Based on these
figures, 300 fewer suicide deaths in England and Wales represent a
potential cost saving of £450 million annually.
- NCISH impact continued during the assessment period (see also wider
and emerging impact). NCISH's 2013 Annual Report (3) showed a 26% fall
in overall patient suicide rates in England (2004-2011). We also
reported sustained improvements in in-patient safety — in-patient
suicide fell by 58% (2001-10) particularly in those who died by hanging
(likely to have been as a result of NCISH recommendation to remove
ligature points). Service changes informed by NCISH research have
continued to be implemented, and two of the recommendations (relating to
crisis teams and dual diagnosis policies) were associated with some the
biggest falls in UK suicide between 1997-2011 — differential falls in
suicide between implementing and non-implementing services of 30% and
12% respectively (S8).
Wider and emerging impact
Safer Care Ltd. (2013) (company number 08598105) (S9) is a social
enterprise formed in response to NHS Trusts requesting our expertise to
address local aspects of patient safety and suicide prevention. We
forecast a £40,000 turnover in the first full year of operation. Through
Safer Care Ltd., NCISH provides: expert scrutiny of individual cases and
service documentation (SUI reports, service policies) identified by
services, identify themes arising from cases, place local services in the
national context and provide a training seminar to all staff about their
local issues and the national picture.
Sources to corroborate the impact
S1. http://www.bbmh.manchester.ac.uk/cmhr/research/centreforsuicideprevention/nci/reports/safety_first_full_report.pdf
S2. https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/216928/Preventing-Suicide-in-England-A-cross-government-outcomes-strategy-to-save-lives.pdf
S3. Suicide Support and Information System. National Suicide Research
Foundation (NSRF), Ireland. http://www.nsrf.ie/reports//Reports_2012/SSISReport2012.pdf
S4. Norwegian Centre for Violence and Traumatic Stress Centre. Report 4
(2011).
http://www.nkvts.no/biblioteket/Publikasjoner/Violence-prevention-in-Norway-Activities-
and-measures-to-prevent-violence-in-close-relationships.pdf
S5. Example of Hansard entry. All mentions of NCISH work available via www.parliament.uk http://www.publications.parliament.uk/pa/cm201212/cmhansrd/cm120110/debtext/120110-0001.htm#12011048000016
S6. NCISH toolkit for mental health services.
http://www.bbmh.manchester.ac.uk/cmhr/research/centreforsuicideprevention/nci/toolkits/
S7. The National Health Service (Quality Accounts) Regulations 2010.
http://www.legislation.gov.uk/uksi/2010/279/contents/madef
S8. Report, Patient suicide: the impact of service change. Forthcoming,
November 28 2013. Available from UoM on request.
S9. Safer Care Ltd. Company number 08598105. Companies House
http://www.companieshouse.gov.uk