Use of biomechanical modelling to develop and commercialise an artificial spinal implant
Submitting Institution
University of NottinghamUnit of Assessment
General EngineeringSummary Impact Type
TechnologicalResearch Subject Area(s)
Medical and Health Sciences: Clinical Sciences, Neurosciences
Summary of the impact
Research into the biomechanics of intervertebral discs at the University
of Nottingham has made a
significant contribution to the development of two medical implants
(Cadisc®- L and Cadisc®-C) by
Ranier Technology Ltd. 226 patients (90% outside the UK) have had this
treatment, which has
outperformed the alternatives by 34% in measured outcomes of reducing
patient disability (ODI),
pain and quality of life (QALY). Consequently, Cadisc® now accounts for
all of Ranier's business.
The company has expanded its workforce to 35 people and has attracted
external investment of
£13M to perform clinical trials and manufacture the product.
Underpinning research
The discs of the lumbar and cervical spine are subject to degenerative
changes caused by ageing
and the stresses of day-to-day life. The resulting loss in disc height and
flexibility and reduced
ability to absorb shock can lead to pain or even tearing or rupturing of
the disc. As one of the most
common causes of back pain, the Chartered Society of Physiotherapy
estimates that: disc
degeneration is estimated to cost the UK economy alone over £12Bn a year;
nearly 2 million
people worldwide are treated for spinal disc defects annually and 50%
require some structure to be
inserted or implanted; over 7 million work days were lost in the UK from
back pain related illness in
2011 and; back pain is the second most common cause of illness and time
off work [4.1].
It is in this area that Dr Donal McNally (Reader in Bioengineering,
University of Nottingham, 2001-current) has focused an important part of
his research. His work has primarily investigated the
internal mechanical behaviour of the intervertebral disc and load transfer
between it and the
adjacent vertebrae.
Between 2002 and 2009 McNally and his team studied the mechanics of the
intervertebral disc
(including the permeability of the cartilage end plate) and variations of
load patterns in the vertebra
after disc implantation. This was done by developing finite element models
of natural and artificial
discs [2.1, 2.4]. The researchers observed an altered stress pattern in
the vertebrae adjacent to
implanted segments and found that the use of smaller-size implants and
presence of voids at the
interface caused localised stress concentration in the endplate and
adjacent spongy bone. The
research [2.4] supported the hypothesis that conventional implants fail to
restore normal loading
patters in the vertebral body and that localised high-stress regions could
be a source of pain and
the reason for the low success rate of traditional total disc
replacements. Other studies [2.2]
focused on examining and quantifying the loading and load transfer between
the intervertebral
discs and the adjacent vertebrae.
Work on Cadisc® began in 2002, when medical device development company
Ranier Technology
began sponsoring three PhD students and a postdoctoral researcher at the
University of
Nottingham, who — led by McNally — have contributed key research to
Cadisc®'s development. An
in vitro investigation of the effect of implantation of Cadisc®-L
(for the lumbar spine), using frozen
human lumbar spines, showed a reduction in axial stiffness while
maintaining disc height and
flexion stiffness — all conducive to preserving the biomechanics of an
implanted spinal motion
segment [2.3]. The research also contributed to the development of Cadisc®
by: investigating the
design and performance of surgical instrumentation; validating the
manufacturing process;
modelling the performance of Cadisc®-C for the cervical spine [2.5];
analysis of load transmission
from vertebrae to implant [6]; and confirmation of the biofidelic
performance of the device.
The work is highly multidisciplinary and has involved collaboration with:
spine surgeons (Arun,
Freeman and Mullholland at Nottingham, Fairbank and Meir at Oxford) to
understand better the
surgical needs specific to spine surgery and ease of operation;
orthopaedic surgeon (Scammel at
Nottingham), to appreciate the general surgical situation; physicists
(Gowland and Cox at
Nottingham) to aid with imaging and measurement techniques to evaluate the
pre and post-surgery
conditions; physiologists (Jones and Urban at Oxford) to understand the
human physiology
aspects.
The award of the International Society for the Study of the Lumbar Spine
(ISSLS) Prize — one of
the most prestigious awards in spinal research — in two of three
categories in 2009 demonstrates
the internationally leading quality of the research produced by McNally
and his group [2.5, 2.6].
References to the research
References (Items marked with an asterisk indicate 3 most significant
papers);
2.1. Riches, P.E. and McNally, D.S., 2005, A one-dimensional theoretical
prediction of the effect of
reduced end-plate permeability on the mechanics of the invertebral disc, Proceedings
of the
Institute of Mechanical Engineers, Part H — Journal of Engineering in
Medicine, 219(H5), 329-335 DOI: 10.1243/095441105X34365
2.2. McNally, D.S., 2002, The objectives for the mechanical evaluation of
spinal instrumentation
have changed, European Spine Journal, 11, 179-185 DOI:
10.1007/s00586-002-0435-5
2.3. McNally, D., Naylor, J. and Johnson, S., 2012, An in vitro
biomechanical comparison of
Cadisc®-L with natural lumbar discs in axial compression and sagittal
flexion, European Spine
Journal, 21(5) 612-617 DOI: 10.1007/s00586-012-2249-4
2.4. *Palissery, V., Mulholland, R.C.M. and McNally, D.S., 2009, The
implications of stress patterns
in the vertebral body under axial support of an artificial implant, Medical
Engineering and
Physics, 31, 833-837 DOI: 10.1016/j.medengphy.2009.03.010
2.5. *Meir, A., Fairbank, J.C.T., Jones, D.A., McNally, D.S. and Urban
J.P.G., 2007, High
pressures and asymmetrical stresses in the scoliotic disc in the absence
of muscle loading,
Scoliosis, 2 (4) DOI: 10.1186/1748-7161-2-4
2.6.*Arun, R., Freeman, B.J.C., Scammel, B.E., McNally, D.S., Cox, E. and
Gowland, P., 2009,
What influence does sustained mechanical load have on diffusion in the
human intervertebral
discs? An in-vivo study using serial post-contrast magnetic resonance
imaging, Spine, 34(21),
2324-2337 (2009 ISSLS Prize winner) DOI: 10.1097/BRS.0b013e3181b4df92,
copy available
on request.
Details of the impact
The underpinning research validates the biomedical function of the
Cadisc® implants, which
underwent clinical trials on 30 patients from October 2009 to June 2010
[4.2] and has since led to
the impacts described below.
Patient health benefits
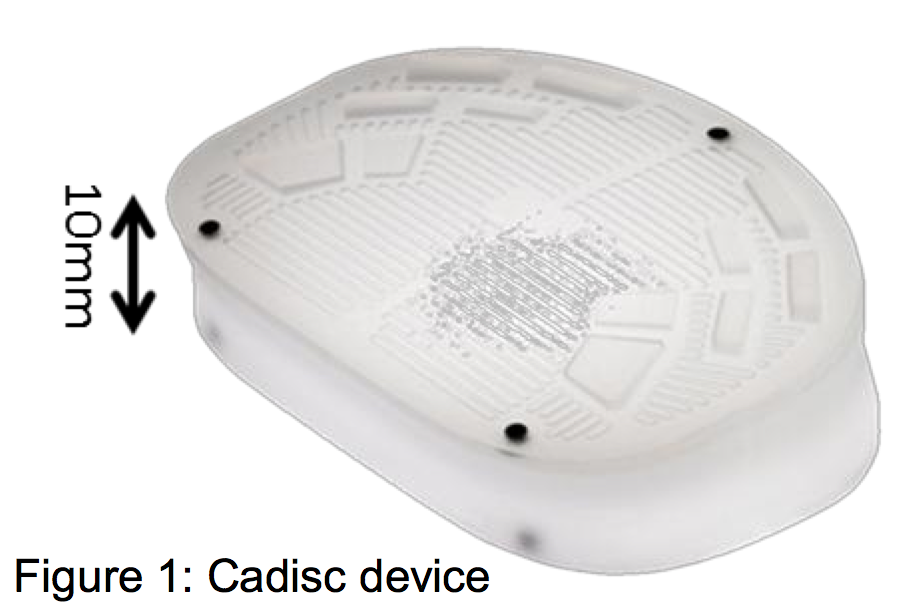
The research has led to the development of two products that are
specifically designed to treat
patients suffering from degenerative disc disease — Cadisc®-L, which
mimics the biomechanical
properties of the natural lumbar disc, and
Cadisc®-C, which does the same for the natural
cervical disc. Based on the research insights
into the mechanical loading on spinal discs and
the transfer of fluid, Cadisc® (see Figure 1) is
designed to replicate the behaviour of a real
spinal disc and hence give better results in
terms of pain relief, mobility and quality of life to
patients soon after surgery. It is unique in that it
does not have a metal endplate and therefore
conforms to vertebral anatomy better than conventional implants [4.3].
The graph below left shows the improvement in Quality Adjusted Life Years
(QALY, a standard
measure of disease burden including both quality and quantity of life) in
the 24 months after
patients received the product, in comparison to alternative treatments
available. QALY accrual rate
for Cadisc® is 0.7 over 12 months, which is approximately twice that of
conventional disc
replacements and three times that of spinal fusion, the current "Gold
Standard" of care [4.4].
In the UK the National Institute for Health and Care Excellence (NICE)
values 1 QALY at £20k to
£30k [4.4]. Using this methodology, the intervention already brings a
value of around £30k to £45k
over the first two years after the intervention per patient.
![Figure 2: Performance of Cadisc® against competition against QALY’s and ODI over time [4.4, 4.6] Figure 2: Performance of Cadisc® against competition against QALY’s and ODI over time [4.4, 4.6]](getImage.aspx?ID=308) Figure 2: Performance of Cadisc® against competition against QALY’s and ODI over time [4.4, 4.6]
Figure 2: Performance of Cadisc® against competition against QALY’s and ODI over time [4.4, 4.6]
Under the Oswestry Disability Index (ODI), one of the principal
condition-specific outcome
measures used in the management of spinal disorders, Cadisc® has shown a
33% performance
improvement compared to competitor products and treatments (see Figure 2
right) [4.5, 4.6].
Between October 2009 and the end of July 2013, 226 patients received
these implants; the
operative success rate was 100% [4.3].
In 2011, after the clinical trials for Cadisc®-L, Dick Zeilstra, the
trial's principal investigator,
highlighted the enormous significance of the discs for patient well-being:
"Over 80% of patients
experienced a clinically significant improvement in Oswestry Disability
Index (ODI) scores and
there was an average improvement in ODI scores of 63% at 12 months; this
compares with an
average improvement of 47% in studies of other disc prostheses. Patients
also experienced
remarkable improvement in quality of life, with Cadisc®-L patients
accruing 0.7 of a Quality
Adjusted Life Year (QALY) at 12 months. In recently published trials,
competitor products
demonstrated a mean accrual of 0.14 of a QALY at 12 months and 0.41 at 24
months." [4.5]
The biomechanical advantages of Cadisc® and its ability to mimic the
natural disc, informed by
UoN research, have been commended by Dr. Hamid Afshar, one of the leading
surgeons
specialising in this area: "The Cadisc® concept is very unique — a single
block disc with no metal
components which offers biomechanics similar to the natural disc.
Conceptually, it's the ideal
solution for the spine. Aside from the biomechanical advantages, the
Cadisc® also offers MR and
CT imaging compatibility which allows clear visualisation of the adjacent
skeletal anatomy and
neural tissues. Having nearly 10 years of product development and testing
provides surgeons the
reassurance that the device will meet the mechanical and functional
demands of the spine. The
Cadisc® technology has helped patients become pain free and enable them to
return to work. In
particular, It gives young patients (20-50 years) the opportunity to
return to a more active, pain-free
lifestyle" [4.7].
Commercial benefits
The research directly contributed to the development and sales of
Ranier's two flagship products,
Cadisc®-L and Cadisc®-C. £8M of third-party investment was secured (from
Alliance Trust Equity
Partners (ATEP) and First Ventures) to fund the clinical testing and
European launch in February
2008 [4.8] followed by a further injection of £5M in 2010 by the same
companies [4.3, 4.9]. Both
products, along with their associated surgical instruments, have been
successful in gaining CE
marks and have been sold commercially throughout Europe since 2009. An
application for an IDE
clinical study was submitted to the US Food and Drug Administration (FDA)
on June 27th 2011
with a view to marketing the devices in the USA and is pursuing further
funding to enable full scale
clinical trials to obtain full FDA approval. Distribution contracts were
signed in early 2013 to cover
the supply of products to the surgical community in South Africa,
Australia and New Zealand [4.10
a&b].
The research has transformed Cambridge-based Ranier Technology from a
small medical device
development company into the only UK manufacturer of total disc
replacements. Cadisc® now
accounts for all of the company's business. It has gained international
reach, exporting 90% of its
production, mainly to Germany. Since 2008 its workforce has grown to 35,
and its turnover has
increased by more than 80% between 2008 and 2013 [4.3].
Sources to corroborate the impact
4.1 http://www.csp.org.uk/documents/impact-nhs-reforms-musculoskeletal-physiotherapy-health-social-care-bill-lords-report-stag
pdf available on file.
4.2 http://clinicaltrials.gov/ct2/show/NCT00949936?term=Cadisc®+Ranier&rank=1
4.3 Dr Geoffrey Andrews, Director, Ranier Technologies Ltd. (letter dated
22nd August 2013)
4.4 Ian Quirk, Cadisc®™ EU Clinical Trials Current Status, Presentation
to the scientific advisory
board of Ranier Technologies, January 2013. Copy available on request.
4.5 http://www.cambridgenetwork.co.uk/news/ranier-announces-results-of-its-Cadisc®-l-lumbar-disc/
4.6 Quirk, I, Bertagnoli, R, Conix, B, Freeman, BJC, Hes, R, and
McConichie, A: Clinical
performance and quality of life following Cadisc®-L total disc
replacement: a prospective, non-randomised, multi-centre trial with 12
months follow-up, ISASS Meeting, Barcelona, 2012
4.7 Mr. Dr. Hamid Afshar, statement available on request. Statement
received via Scott Johnson,
Technical Director, Ranier Technologies Ltd.
4.8 http://www.prnewswire.com/news-releases/ranier-technology-secures-gbp8m-funding-for-its-Cadisc®-replacement-spinal-discs-56961057.html
4.9 https://www.orthoworld.com/knowent/ranier_091010.pdf
4.10a http://www.ranier.co.uk/index.php?public/news-and-events/news/view/ranier-technology-announces-approval-for-reimbursement-in-south-africa-for-Cadisc®-c-compliant-elastomeric-artificial-disc
4.10b http://www.ranier.co.uk/index.php?public/news-and-events/news/view/ranier-signs-with-distribution-partner-asdm-in-australia-for-lumbar-and-cervical-discs