Incorporating empathy in training standards for healthcare professionals
Submitting Institution
University of GlasgowUnit of Assessment
Public Health, Health Services and Primary CareSummary Impact Type
HealthResearch Subject Area(s)
Medical and Health Sciences: Public Health and Health Services
Summary of the impact
The ability of healthcare professionals to empathise with patients has
been shown to enhance patient satisfaction, improve symptoms and promote
well-being. Research at University of Glasgow has developed the
Consultation and Relational Empathy (CARE) Measure — the first validated,
patient-rated questionnaire developed in a primary care setting that
measures patient perceptions of healthcare professionals' empathy and
quality of care. The CARE Measure is formally embedded into healthcare
professional training standards through its inclusion in Scottish General
Practitioner (GP) appraisals and the Royal College of General
Practitioners Membership (MRCGP) and Interim Membership by Assessment of
Performance (iMAP) processes; through these means more than 8,000 GPs are
using the CARE Measure. It has also been incorporated into the Scottish
Government's policy on Healthcare Quality and adopted by the General
Medical Council and the Chartered Society of Physiotherapy.
Underpinning research
Empathy is recognised as a vital interpersonal skill that enables
healthcare professionals to provide optimal care for patients.1
Between 2000 and 2003, Mercer led the development and validation of a
novel and suitable tool to assess clinician empathy; the Consultation and
Relational Empathy (CARE) Measure. The research steps undertaken between
2000-2003 were:
Firstly, following an extensive literature review, Mercer highlighted the
importance of empathy in healthcare, whilst confirming a lack of validated
measures suitable for use in primary care1. Secondly, Mercer
led the initial development and preliminary validation of the CARE Measure
in primary care.2 An important aspect of this was the
collaborative approach taken to the measure's development and testing,
which involved patients and practitioners from both high and low
socioeconomic deprivation areas.2 The aim of developing the
measure in this manner was to ensure it was meaningful to all patients,
irrespective of their deprivation level, which was deemed to be important
given the wide health inequalities that exist in Scotland and indeed the
UK. Thirdly, Mercer led a major study on more than 3,000 patients (again
in areas of high and low deprivation) which confirmed the validity and
reliability of the CARE Measure in General Practice, and its ability to
effectively discriminate between qualified GPs; thus establishing
its utility in GP assessment.3 This research, carried out at
the University of between 2000-2003 and published in international
peer-reviewed journals, laid the academic foundation for the subsequent
adoption of the measure `by RCGP Scotland for use in GP Appraisal. The
utility of the CARE Measure in assessment of GPs in training was
then established in research led by Murphy and colleagues at NHS Education
for Scotland, (NES) in collaboration with Mercer.4 On the basis
of this cumulative research, the CARE Measure was subsequently adopted as
part of work-based assessment of GPs in training in the UK.
The utility of the CARE Measure in secondary care was established between
2003-2008 in work led by Mercer in collaboration with Murphy and others.5,6
This established validity of the measure in both primary and secondary
care.
Since 2008, the CARE Measure has been validated in other professional
groups, including Nurses and a wide range of Allied Health professionals.
The work is funded by the Scottish Government and led by Dr Edward Duncan
at Stirling University, in collaboration with Mercer. Publications are in
preparation.
Key University of Glasgow Researchers
Stewart Mercer (Clinical Fellow, [2000-2003]; Senior Clinical Fellow
[2003-2008], now Chair in Primary Care Research) led the development of
the CARE Measure; Professor Graham Watt Professor of General Practice
[1994-present]) provided mentoring input, but did not have specific
expertise in questionnaire design or validation. He was a co-author on two
publications.2,3 Alex McConnachie (Consultant Statistician
[1996-2008]) provided statistical expertise in one publication.3
Key External Collaborators
Dr Margaret Maxwell and Dr David Heaney (both University of Edinburgh),
gave advice on the methodology of validation of the CARE Measure between
2000-2003. They were co-authors on two of the CARE Measure publications.2,3
Douglas Murphy (University of Dundee) was involved in work on GPs
in training.4 Mercer led the validation work in secondary care,
with input from Murphy on the statistical analysis.5,6 Dr
Edward Duncan (The Nursing, Midwifery and Allied Health Professions
Research Unit, University of Stirling) was the Principal Investigator on a
Scottish Government funded project, involving University of Glasgow, to
validate the CARE Measure in other professional groups. Publications are
in preparation.
References to the research
Details of the impact
Practitioner empathy involves an ability to understand the patient's
situation, perspective and feelings, the capability to communicate and
confirm this with the patient, and subsequently apply this understanding
in a therapeutic manner. Before 2000 there were no validated measures to
assess empathy that were suitable for use in routine healthcare across a
range of settings. Research at University of Glasgow has developed the
first validated patient-rated questionnaire in a primary care setting that
measures patient perceptions of healthcare professionals' empathy and
quality of care for general practice.
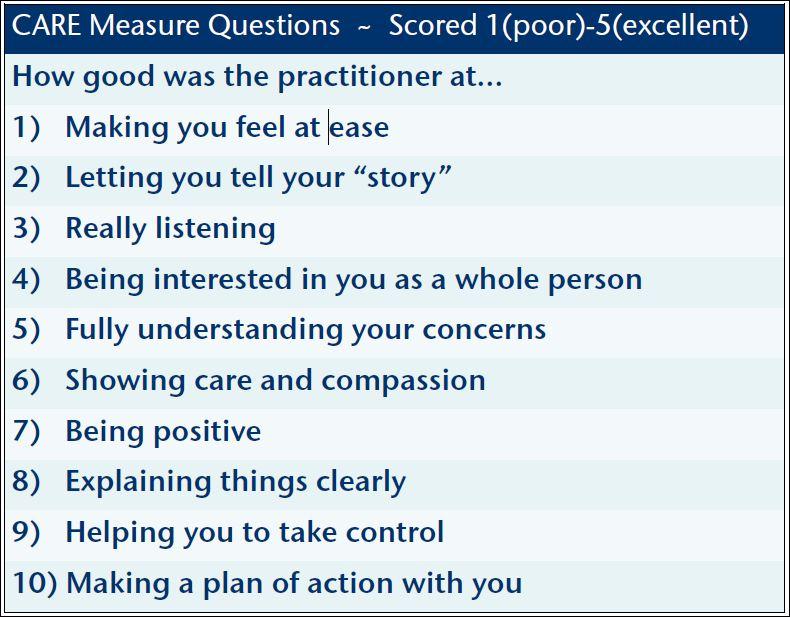
The CARE Measure is freely available to download from the University of
Glasgow website.a The image to the right illustrates the
questions involved in the measure. Since 2004, the CARE Measure has formed
an integral component of professional bodies and government initiatives
(details of which are provided below):
- RCGP professional training standards, to facilitate assessment,
appraisal and revalidation
- Scottish Government policy on Healthcare Quality
- Chartered Society of Physiotherapy patient experience reporting
In addition, funding was provided by the Scottish Government to establish
a website in 2012 as part of the validation work in Allied Health
Professionals, led by Duncan in collaboration with Mercer.b
This website facilitates the collection and use of CARE Measure data from
medical, Nursing and Allied Health Professional practitioners, allowing
registered users to compare their data with that of their peers, to
identify any potential areas of improvement. Between going live in
September 2012 and 31st July 2013, there were 1180 registered
users, primarily doctors.c
Incorporation of the CARE Measure in RCGP professional training
standards to facilitate assessment, appraisal and revalidation
The MRCGP exam is a compulsory assessment system that complies with the
standards set by the UK's GMC. It confirms a doctor's competence in the
speciality of General Practice and ability to practice independently in
the UK. Completion of the MRCGP is a pre-requisite for the certificate of
completion of training (CCT) and full RCGP membership. Since August 2007,
the CARE Measure (renamed Patient Satisfaction Questionnaire (PSQ) by the
RCGPd) has been used as a compulsory evidence-based tool in the
Workplace-Based Assessment component of the MRCGP Exame. In
this capacity, the PSQ allows patient feedback to be gathered on empathy
and relationship-building with each GP trainee. Two cycles of the PSQ are
used during the training period: once in GP placement in Speciality
Training year 1 or year 2 and once in Speciality Training year 3.e
The RCGP estimates that with approximately 3,000 GP trainees each year, an
average of 33,000 cycles of PSQ were completed by trainees between 1st
Jan 2008 and 31st July 2013.e The decision by RCGP
to adopt the CARE Measure was based on its proven ability to effectively
discriminate between doctors [references 3 and 4, above].
iMAP is the process whereby independent practitioners on the GP register
may become members of the RCGP. Assessment for membership on this basis
requires the completion of fifteen compulsory modules, one of which
specifically addresses the PSQ. The PSQ was initially the only tool to
facilitate this when iMAP was launched in 2007.f It is now one
of seven tools approved; encouraging its uptake, it is the only tool
available free of charge.g The RCGP estimates that since 2007,
approximately 30% of applicants to iMAP used the PSQ.f The
decision by RCGP to adopt the CARE Measure was based on its proven ability
to effectively discriminate between doctors [references 3 and 4, above].
Revalidation is the process by which all 60,000 licensed doctors must
demonstrate to the GMC that they are up to date and fit to practice; this
ensures compliance with the relevant professional standards, and is thus
compulsory to maintain a license to practice. To determine its suitability
for use in revalidation, the CARE Measure has twice been comprehensively
reviewed by the RCGP; in 2009 it was one of nine patient feedback tools
reviewed,h and in 2010 it was one of ten reviewed.h
Subsequently, the CARE Measure has been fully endorsed by RCGP as a `fit
for purpose' patient survey for use in the revalidation process.h,i
The CARE Measure is used by GPs in Scotland as both a patient satisfaction
survey and for appraisal and revalidation; it is listed in the Scottish
Online Appraisal Resource (the key online information point for GP
Appraisal).j,k Since 2004, it has been accredited for use in
appraisal of all GPs in Scotland.l The decision by the GMC to
adopt the CARE Measure was based on its proven ability to effectively
discriminate between doctors [references 3-6, above].
Implementation of the CARE Measure into government policy
In Scotland, the CARE Measure is detailed in the Government's Quality
Strategy (2010).m The Quality Strategy aims to allow those
involved in Scotland's healthcare — namely all healthcare professionals
(numbering 100,000), partners and the public — to work towards achieving
three Quality Ambitions of Safe, Person-Centred and Effective healthcare.
The Quality Strategy specifies the use of the CARE Measure as a tool to
capture patients' assessments of their relationships with healthcare
professionals, allowing an understanding of health outcomes and patient
experience to be determined, and for improvement to be informed where
required.m Inclusion of the CARE Measure has made Scotland the
first country in the world to include staff empathy as a component of
healthcare quality. The decision by the Government to adopt the CARE
Measure was based on its proven ability to effectively discriminate
between practitioners [references 3-6, above], and by a series of
high-level meetings and discussion between Mercer and the Scottish
Government between 2009-2010, including the Chief Executive of NHS
Scotland at the time (Dr Derek Feeley) and the then Cabinet Secretary and
Minister for Health, Nicola Sturgeon.
Implementation of the CARE Measure as a validated Patient
Reported Experience Measure
Since 2012, the Chartered Society of Physiotherapy has recommended the
CARE Measure to their 52,000 members (98% of UK physiotherapists).n
In this context, the CARE Measure is being used by the Chartered Society
of Physiotherapy as the primary validated Patient Reported Experience
Measure, to assess and improve Physiotherapy services along with the
overall patient journey.n The CARE Measure became a
recommendation after a 2009 Scottish pilot study (collaboration between
University of Glasgow and University of Stirling) associated with
Physiotherapy training and person centred care, which subsequently led to
involvement in validation work in Allied Health Professionals.
Sources to corroborate the impact
a. CARE
Measure, University of Glasgow webpage
b. CARE Measure Website
c. Evidence to substantiate available on request (Organisation: CARE
Measure.org)
d. PSQ
Form, RCGP
e. Evidence to substantiate available on request (Organisation: RCGP)
f. Evidence to substantiate available on request (Organisation: RCGP)
g. iMAP
Handbook, RCGP, April 2013
h. Evidence to substantiate available on request (Organisation: RCGP)
i. Patient
feedback tools `fit for purpose', RCGP
j. Scottish
Online Appraisal Resource Guidance (p18), RCGP Scotland
k. Guidance
on revalidation, RCGP Scotland
l. Evidence to substantiate available on request (Organisation: RCGP
Scotland)
m.
The Healthcare Quality Strategy for NHS Scotland (May 2010)
n. Evidence to substantiate available on request (Organisation: Chartered
Society of Physiotherapy)