Reducing unnecessary attendance at hospital emergency departments by improving care out of hospital
Submitting Institution
Swansea UniversityUnit of Assessment
Allied Health Professions, Dentistry, Nursing and PharmacySummary Impact Type
HealthResearch Subject Area(s)
Medical and Health Sciences: Nursing, Public Health and Health Services
Summary of the impact
Care provided to patients by emergency ambulance services is changing
nationally and internationally. For example the proportion of 999 calls in
England resulting in conveyance to hospital fell from 68% in 2007-8 to 55%
in 2012-3. Professor Snooks of Swansea University and colleagues have
collaborated with clinicians, policy makers and academics to identify
approaches more cost-effective than routine conveyance to Emergency
Departments (EDs) for many patients. International application of Snooks's
evidence that telephone advice, decision support and referral pathways are
safe and effective has reduced unnecessary attendance at EDs and costs
without compromising patient experience, safety or quality of care.
Underpinning research
Calls to emergency health services continue to rise internationally. In
England there were 9.1 million calls in 2012-13 — 80% more than in
2002-03. Most calls are neither life-threatening nor serious: in 2002 a
review led by Snooks, Senior Lecturer in Health Services Research at
Swansea University since the start of 2000 (Professor from 2006), reported
that 40% of calls to emergency health services world-wide did not need an
emergency ambulance [R1]. This unnecessary workload jeopardises timely
responses to those with urgent needs, thus causing avoidable morbidity and
mortality across the spectrum of need.
Between 2000 and 2013, Snooks and her team at Swansea University have
undertaken a programme of applied research in collaboration with ambulance
service providers, policy makers and academics to identify safe and
cost-effective alternatives to ambulance dispatch and conveyance to ED.
Supported by over £4 million in research grants from peer-reviewed
national programmes [R10-R12], the research has included systematic
reviews, cohort studies and randomised trials aimed at improving triage
and decision-making in emergency care out of hospital, including new
protocols and pathways for referrals to non-emergency healthcare
providers. The work has included three main internationally relevant
themes:
A Observational studies by Swansea University (2003-6) analysed existing
UK emergency care practice and outcomes to inform future development.
Analysis of outcomes in people aged 65 or over who were left at home by an
ambulance crew after a fall showed that current practice is unsafe for
patients, with about half making at least one further emergency healthcare
contact within 2 weeks, and fivefold increases in risk of emergency
admission and of death [R2]. These findings were reinforced by reviews and
focus-group studies [R3].
B Swansea University led, or made major contributions to, experimental
evaluations of alternatives to ED conveyance that enable
paramedics to leave patients at home with referral to a non-emergency
health care provider. In 1999-2001, ending after Snooks arrived in
Swansea, we developed and tested 23 `Treat and Refer' protocols for
ambulance crews to assess patients on scene and, when appropriate, use
alternative pathways of care to avoid hospital admission. Findings from
this controlled before-and-after study were encouraging but not
definitive: the intervention was generally acceptable to 250 intervention
patients and crews but the conveyance rate to ED remained unchanged [R4].
The Paramedic Practitioner Older People Study (2003-5) was a randomised
trial showing that paramedics with extended clinical skills (e.g.
suturing) could avoid standard ambulance transfer to ED for patients aged
over 60 with acute minor conditions, and improve both subsequent emergency
contacts and patient satisfaction [R5, R10]. The SAFER 1 randomised trial
(2006-11) evaluated the effect of a computerised clinical decision support
tool on the care of older people who had fallen; it found that the new
model of care was safe, doubled referrals to community falls services, and
was potentially cost-effective [R6, R11].
C Experimental evaluations by Swansea University and collaborators of alternatives
to ambulance dispatch at initial telephone contacts with the
health service included a randomised trial of computerised decision
support for 999 call takers (1998-2000, ending after Snooks arrived in
Swansea). This showed the safety of telephone assessment and advice in
place of sending an ambulance to patients with problems triaged as
non-serious [R7], and stimulated reductions in emergency ambulance
dispatch rates without increasing risk: 330 of 635 intervention group
patients (52%) were triaged as not requiring an emergency ambulance [R8].
A further study (2002-2006) showed the safety and potential effectiveness
of provision of advice to callers to the emergency ambulance service by
nurses through National Health Service (NHS) Direct: in only 4 of 1552
cases identified could delay in sending an ambulance have been clinically
important [R9].
References to the research
Journal Impact Factors (JIFs) and Scopus citations accessed in October
2013
R1. Snooks H et al. NHS emergency response to 999 calls:
alternatives for cases that are neither life threatening nor serious. BMJ
2002;325:330. DOI:10.1136/bmj.325.7359.330
(JIF = 17.2; 34 citations).
R2. Snooks H et al. Emergency care of older people who
fall. Qual. Saf. Health Care 2006;15:390-2. DOI:10.1136/qshc.2006.018697
(JIF = 2.8; 25 citations).
R3. Porter A, Snooks H et al. `Should I stay or should I
go?' Deciding whether to go to hospital after a 999 call. J. Health
Serv. Res. Policy 2007;12 (Suppl. 1):32-8. DOI:10.1258/135581907780318392
(JIF = 1.6; 7 citations).
R4. Snooks H et al. Towards primary care for
non-serious callers to emergency ambulance service: results of controlled
study of `Treat & Refer' protocols for ambulance crews. Qual. Saf.
Health Care 2004:13:435-43. DOI:10.1136/qshc.2003.007658
(JIF = 2.8; 14 citations).
R5. Mason S, Snooks H et al. Effectiveness of paramedic
practitioners for older people: results of a cluster randomised controlled
trial. BMJ 2007:335:919-23. DOI:10.1136/bmj.39343.649097.55
(JIF = 17.2; 31 citations).
R6. Snooks H et al. Support & Assessment for Fall
Emergency Referrals (SAFER 1): evaluation of costs & benefits of
computerised decision support for emergency ambulance personnel to plan
appropriate care for older people who have fallen. London:
Department of Health; 2011. http://tinyurl.com/nye4v7k.
R7. Dale J, Snooks H et al. Computer assisted assessment
and advice for "non-serious" 999 ambulance service callers: the potential
impact on ambulance despatch. Emerg. Med. J. 2003;20:178-83.
http://tinyurl.com/oq8b2wt (JIF =
1,6; 23 citations).
R8. Dale J, Snooks H et al. Safety of telephone
consultation for `non-serious' emergency ambulance service patients. Qual.
Saf. Health Care 2004;13:363-73. DOI:10.1136/qshc.2003.008003
(JIF = 2.8; 29 citations).
R9. Turner J, Snooks H et al. The costs and benefits of
managing low priority 999 ambulance calls by NHS Direct nurse advisors.
London: NIHR Service Delivery and Organisation Research Programme; 2006. http://tinyurl.com/oqrnxq6.
Selected peer-reviewed research grant support
R10. Randomised trial to evaluate the effectiveness of Paramedic
Practitioners managing Older People calling 999 with minor conditions.
Private Patients Plan Foundation, 2002-5, £260,000; Snooks co-applicant.
R11. Support and Assessment for Fall Emergency Referrals (SAFER 1):
evaluation of costs and benefits of on-scene computerised decision support
for emergency ambulance personnel to assess and plan appropriate care for
older people who have fallen. Department of Health, 2006-11, £570,000;
Snooks lead applicant. http://tinyurl.com/oqlpthm.
R12. Evaluation of cost-effectiveness of passing non-serious 999 calls to
NHS Direct for management. NHS Executive Service Delivery and Organisation
research programme, 2002-6, £380,000; Snooks co-applicant and lead for
Welsh site.
Details of the impact
The programme of research, dissemination and service support by
Swansea University and collaborators has provided scientific foundation
for major changes in conveyance to hospital by emergency ambulances. In
England, for example, the proportion of emergency calls leading to
hospital conveyance has fallen from 68% (4.3 million of 6.3 million in
2007-8 to 55% (5.0 million of 9.1 million in 2012-3 (Figure 1). Though
causal inference in this multifactorial field is difficult, we estimate
that hospital conveyances in 2012-3 were some 1.2 million fewer than
expected if the pattern of 2007-8 had continued. If the cost of these
avoided ambulance journeys alone is calculated, at £20 per journey
(source: NHS unit costs), we estimate the marginal benefit of the journeys
avoided as £24 million. These reduced attendances at ED are very likely to
yield even more savings for the NHS, but the value of these is more
difficult to estimate.
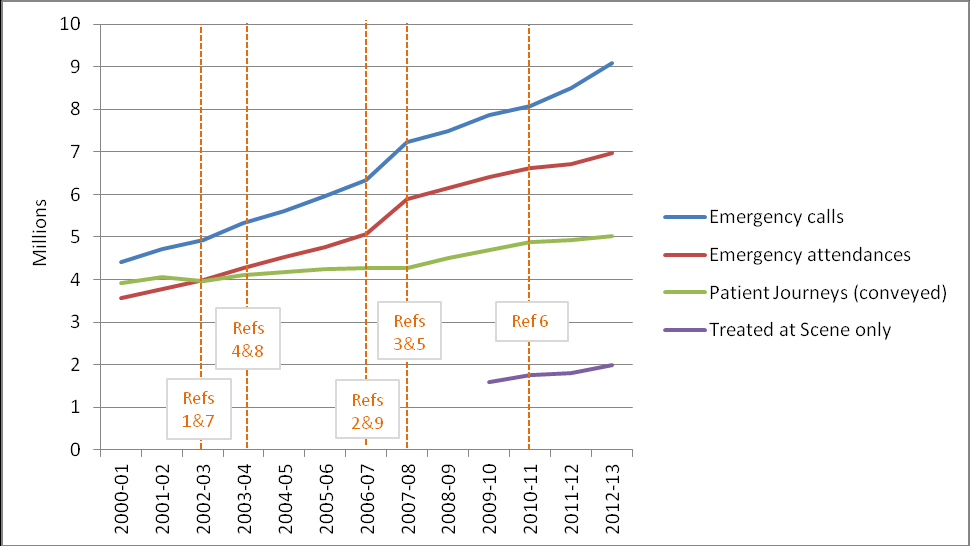 Figure 1: 999 calls and consequences 2000-13 (source NHS Information Centre)
Figure 1: 999 calls and consequences 2000-13 (source NHS Information Centre)
Snooks's leadership in this field is exemplified by her initiation of,
and continued engagement with, the 999 Emergency Medical Services Research
Forum and the Thematic Research network for emergency, UnScheduled and
Trauma care (TRUST) (http://www.trustresearch.org.uk/en/);
both link service providers and researchers in setting emergency care
research priorities and promoting evidence-based policy and practice.
Swansea University and collaborators have achieved impact on patient
care, service efficiency and staff development not only in the UK but also
internationally, notably across Australia and Canada. The results of our
research have been used during the development of strategies, guidelines
and standards issued by governing bodies including the Department of
Health, Welsh Government, NHS Scotland and authorities in Victoria,
Australia and Alberta, Canada [C6-C11]. That this research has achieved
impact on policy, service delivery and patient experience over 2008-13, is
also recognised by key people in this field:
"Professor Snooks's work was used in the strategic review of NHS
Ambulance Services in England [C7], the catalyst for transforming
ambulance services over the last seven years ... to modernise services,
professionalise staff, and provide care that is more efficient for the
NHS and appropriate for patients, whilst maintaining safety standards."
[C1]
"Snooks's studies, at the forefront of pre-hospital research, have
significantly influenced the development of new models of ambulance
service care ... including the development of alternatives to ambulance
conveyance, telephone triage, and the safe management of falls. This
work in turn has influenced national policy on reorganisation of
delivery models for ambulance and pre-hospital health care." [C2]
Ambulance service providers across UK have implemented phone-based advice
in accordance with recommendations from the Department of Health in
response to our research. For example NHS Direct nursing staff at several
sites now provide advice to Category C emergency callers, the least
urgent. In 2012-13 over 360,000 emergency calls in England were resolved
through telephone advice, avoiding ambulance dispatch (source: NHS
Information Centre).
Our work on the development and evaluation of `Treat and Refer' protocols
and extended paramedic roles has prompted all UK ambulance services to
introduce pathways for ambulance crews to assess patients for alternatives
to hospital admission. We are aware of similar service models being
adopted internationally, for example in Australia and Canada:
"Snooks's work, including evidence of caller satisfaction and very few
adverse events from referrals instead of conveyance, supported
implementation of a point-of-call referral service in Victoria. The
model is being rolled out across Australia." [C3]
"The change from routine dispatch of an ambulance for every call
resulted in the referral of 40,000 callers in the state of Victoria to
alternative care in 2012-3, thus increasing availability of ambulances
to respond to emergency calls." [C11]
"In Alberta, Canada we have developed and implemented models of care
that avoid automatic transportation of 911 patients, based on Snooks's
innovative work on `Treat and Refer' and we have introduced extended
training for paramedics to make decisions about who goes to hospital and
who is best left at home with a community-based care referral." [C4]
"Professor Snooks's study findings have been used to support the
development and implementation of new services including: (1) Since
2009 paramedic-nurse teams have staffed rural EDs, assessing and
treating patients overnight with on-call physician support;
(2) Since 2009 advanced paramedics and nurses have staffed our
dispatch center, providing advice to field paramedics, and coordinating
emergency calls and inter-facility transfers;
(3) Since 2011 advanced paramedics have responded to calls at nursing
homes, delivering emergency care at the bedside & avoiding
unnecessary transport to emergency depts." [C5]
Hence translating the research by Swansea University and our
collaborators into practice has achieved impact across many countries,
with benefits to patients, their families, and healthcare providers by
identifying safe alternatives to conveyance to hospital by emergency
ambulance for those without immediate care needs [C12].
Sources to corroborate the impact
Personal corroboration / statement
C1. Chief Executive, St John, New Zealand. (Formerly) National Ambulance
Director, Department of Health (2004-2012); Chief Executive, London
Ambulance Service (2000—2012) and National Advisor to Department of Health
for Ambulance Services.
C2. Associate Clinical Director and Research Lead, East Midlands
Ambulance Service NHS Trust; and Chair National Ambulance Research
Steering Group.
C3. Senior Intensive Care Paramedic, Ambulance Victoria, Australia.
C4. Senior Performance Strategist, Alberta Health Services Emergency
Medical Services; and Chair of Alberta Health Services Emergency Medical
Services Research Committee, Canada
C5. Research Leader, Nova Scotia Emergency Health Services, Canada.
Relevant policy documents
C6. Department of Health. Taking healthcare to the patient:
transforming ambulance services. London: DH; 2005. http://tinyurl.com/p4zkz87
[underpins Statements 1, 2]
C7. NHS England. High quality care for all, now and for future
generations: Transforming urgent and emergency care services in England.
The Evidence Base from the Urgent and Emergency Care Review.
DH:2013.http://tinyurl.com/mw9bn2t.
[underpins Statements 1, 2]
C8. Welsh Assembly Government (WAG). Guide to good practice:
emergency care — tools and techniques to enable the NHS and Social
Services to improve the delivery of health and social care. Cardiff:
WAG; 2004.
C9. NHS Scotland. Shifting the balance of care: good practice and
research. http://tinyurl.com/p6r797j.
C10. Ambulance Victoria. 2012-2013 Annual Report. http://tinyurl.com/nrjmmjw
[underpins Statement 3]
C11. Government of Alberta and Alberta Health Services. Becoming the
best: Alberta's Health Action Plan 2010-2015.; 2010. http://tinyurl.com/2dmlthb.
[underpins Statement 4]
Publication
C12. Snooks HA. et al. New models of emergency prehospital care
that avoid unnecessary conveyance to Emergency Department: translation of
research evidence into practice? The Scientific World Journal
2013;182102. dx.doi.org/10.1155/2013/182102