UOA01-24: Revolutionising the Treatment of Rheumatoid Arthritis
Submitting Institution
University of OxfordUnit of Assessment
Clinical MedicineSummary Impact Type
EconomicResearch Subject Area(s)
Medical and Health Sciences: Clinical Sciences, Immunology
Summary of the impact
Rheumatoid arthritis is a debilitating inflammatory condition, affecting
around 500,000 people in the UK and around 0.5-1% of the adult population
worldwide. Using novel techniques to study human synovium, Professor Sir
Marc Feldmann and Professor Sir Ravinder Maini from the Kennedy Institute
of Rheumatology identified a therapeutic target, TNFα, for treatment of
rheumatoid arthritis. Following successful clinical trials, showing the
safety and effectiveness of this new target, anti-TNFα antibodies have now
become the gold standard treatment for severe rheumatoid arthritis
worldwide. In addition to dramatically impacting patient care, anti-TNFα
antibodies represent the largest group of therapies against rheumatoid
arthritis on the market, with annual sales currently exceeding US$24.4
billion.
Underpinning research
Since the late 1980s disease-modifying antirheumatic drugs (a term used
to describe several medications, which reduce the rate of damage to bone
and cartilage) have been widely used to decrease disease activity and
prevent joint damage in patients with rheumatoid arthritis. However, many
of these drugs have been known to cause serious side effects, such as low
white blood cell counts and liver damage. After testing his hypothesis
that antigen presentation and cytokines were important in autoimmunity1
Professor Sir Marc Feldmann first identified tumour necrosis factor alpha
(TNFα) as a key therapeutic target for rheumatoid arthritis in 19832.
In 1992, Professor Feldmann, his colleague Professor Maini, and their team
embarked on a number of significant studies and clinical trials, using
monoclonal antibodies against TNFα. These trials showed that inhibition of
TNFα was safe and rapidly effective, and led to the development and
commercialisation of anti-TNFα as a treatment for rheumatoid arthritis,
first approved in 1998 in the US.
The first clinical study, performed at Charing Cross Hospital in 1993,
enrolled 20 patients who had previously shown resistance to all existing
treatments. After giving them an infusion of cA2, a monoclonal antibody to
TNFα, now termed "Infliximab", patients experienced a dramatic improvement
in their symptoms and signs. These results led to a randomised
placebo-controlled trial in collaboration with three other European
centres. The response rate with the highest dose of infliximab was 79% at
4 weeks in comparison to 8% with placebo. The success of repeated
treatments was then demonstrated in a smaller study, however, the duration
of response diminished, partly due to an immune response against the TNFα
antibody itself. Further studies using a mouse model of rheumatoid
arthritis indicated that the combination of an anti-TNF monoclonal
antibody with therapy targeting T cells might improve the effectiveness.
This finding led to the combined use of methotrexate (already established
in the treatment of rheumatoid arthritis) with infliximab, in the next
randomised controlled trial3. The demonstration of synergy with
this combination therapy, without increased toxicity, set the gold
standard for pharmacological management of rheumatoid arthritis.
Additional clinical studies led by the Kennedy Institute showed that
biologic TNFα inhibition plus methotrexate markedly inhibits the
structural joint damage previously thought to be an irreversible feature
of rheumatoid arthritis4. In addition, follow-up studies
demonstrated that TNFα regulates inflammatory cell migration to joints via
modulation of chemokines, adhesion molecules, and joint vascularity5,6.
The primary research underpinning the impact of anti-TNFα took place at
the Kennedy Research Institute between 1993 and 1998. While the Institute
was then based at Imperial College London between 2000 and 2011, the
Kennedy Research Institute remained a separate, freestanding division and
in August 2011 the Kennedy Institute was fully incorporated into the
University of Oxford. Professor Sir Marc Feldmann continues to lead
research into the role of cytokines in disease.
References to the research
1. Bottazzo G.F., Hanafusa T., Pujol-Borrell R., Feldmann M. Role of
aberrant HLA-DR expression and antigen presentation in the induction of
endocrine autoimmunity. Lancet 322 (8359):1115-9 (1983). http://dx.doi.org/10.1016/S0140-6736(83)90629-3
First< conception of hypothesis that antigen presentation and its
regulation by cytokines< could be important in the pathogenesis of
autoimmunity.
2. Brennan F.M., Chantry D., Jackson A., Maini R.N., Feldmann M.
Inhibitory effect of TNFα antibodies on synovial cell interleukin-1
production in rheumatoid arthritis. Lancet 334(8657):244-247
(1989). http://dx.doi.org/10.1016/S0140-6736(89)90430-3,
First demonstration that TNFα was a therapeutic target, as blocking
TNF also blocked other proinflammatory cytokines, IL-1 in this case.
3. Maini R.N. et al.Therapeutic efficacy of multiple intravenous
infusions of anti-tumor necrosis factor a monoclonal antibody combined
with low-dose weekly methotrexate in rheumatoid arthritis. Arthritis
Rheum 41:1552-63 (1998). doi:10.1002/1529-0131(199809)41:9<1552::AID-ART5>3.0.CO;2-W.
Paper reporting follow-up randomised controlled trial, which combined the use of
methotrexate with infliximab.
4. Maini R. et al. Infliximab (chimeric anti-tumour necrosis factor a
monoclonal antibody) versus placebo in rheumatoid arthritis patients
receiving concomitant methotrexate: a randomised phase III trial. ATTRACT
Study Group. Lancet 354(9194):1932-39 (1999).
doi:10.1016/S0140-6736(99)05246-0. Reporting findings from
additional clinical studies, showing biologic TNFα inhibition plus
methotrexate inhibits structural joint damage.
5. Taylor P.C. et alReduction of chemokine levels and leukocyte traffic
to joints by tumor necrosis factor alpha blockade in patients with
rheumatoid arthritis. Arthritis Rheum 43:38-47 (2000).
doi:10.1002/1529-0131(200001)43:1<38::AID-ANR6>3.0.CO;2-L. Paper
reporting that TNFα regulates inflammatory cell migration to joints via
modulation of chemokines, adhesion molecules, and joint vascularity.
6. Taylor P.C. et al. Comparison of ultrasonographic assessment of
synovitis and joint vascularity with radiographic evaluation in a
randomized, placebo-controlled study of infliximab therapy in early
rheumatoid arthritis. Arthritis Rheum 50:1107-16 (2004).
doi:10.1002/art.20123. Paper reporting a follow-up study, which
demonstrated that TNFα regulates inflammatory cell migration to joints
via modulation of chemokines, adhesion molecules, and joint
vascularity.
This research was initially funded by the Nuffield Foundation, the
Medical Research Council, and the Wellcome Trust. Over the years the major
funder for non-clinical has been Arthritis Research UK, and for clinical
Centocor, Inc.
Details of the impact
Rheumatoid arthritis is a persistent inflammatory arthritis of synovial
joints that currently affects around 500,000 people in England and an
estimated 0.5-1% of the adult population worldwide. Rheumatoid arthritis
can lead to pain, deformity and loss of function, work disability,
economic losses and premature death. Prior to the development of anti-TNFα
therapies, a considerable proportion of patients treated with the
available disease-modifying antirheumatic drugs (DMARDs) were still
plagued by premature death rates, and had evidence of persistent disease
activity, with many patients remaining wheelchair bound due to ongoing
joint damage and disability.
The commercial introduction of anti-TNFα agents from 1999 has profoundly
changed the management of severe rheumatoid arthritis throughout the
developed world, with over 2 million patients having received this
treatment. Anti-TNFα therapy has had a profound impact on the quality of
life of patients with rheumatoid arthritis. It is capable of not only
controlling symptoms such as pain and stiffness, it can also protect
joints from the structural damage which leads to disability. This has also
prompted the successful use of anti-TNFα therapy in a number of other
immune-inflammatory diseases, such as juvenile rheumatoid arthritis,
ankylosing spondylitis, psoriatic arthritis, Crohn's disease, ulcerative
colitis, and psoriasis. One study on the effects of anti-TNFα therapy in
patients with Crohn's disease showed that it significantly improved the
quality of life of patients, by increasing their ability to work and
participate in leisure activities, decreasing fatigue, depression, and
anger7. In addition, whilst TNF inhibition in established
disease does not result in cure, evidence is emerging that commencing
treatment during early disease can result in drug-free remission8.
The British Society of Rheumatology issued guidelines on the use of
anti-TNFα inhibitors in rheumatoid arthritis in 2001, and the National
Institute for Health and Clinical Excellence endorsed the therapy in 20029.
The combination of an anti-TNFα agent with methotrexate remains
unsurpassed in reducing the signs and symptoms of rheumatoid arthritis and
in improving joint destruction10. Current UK guidelines also
address the optimal use of biologics and disease modifying antirheumatic
drugs (including methotrexate) for the management of rheumatoid arthritis11,
12. The 2010 European League Against Rheumatism guidelines for the
management of rheumatoid arthritis recognise the importance of early
introduction of biologic TNFα inhibitors in patients failing to reach a
treatment target of remission or low disease activity on conventional,
non-biologic synthetic DMARDs13. Anti-TNFα therapy is the
recommended first line treatment, and if therapeutic response is not
achieved within 3-6 months, the guidelines recommend a trial of either a
second anti-TNF agent or a biologic of an alternative mechanism of action13.
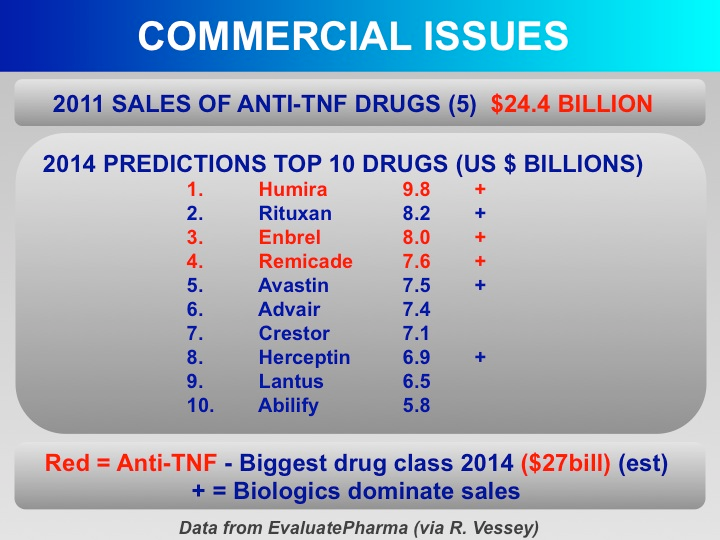
The development of anti-TNFα inhibitors by the Kennedy Institute has had
a major impact on the pharmaceutical industry. Sales of the five licensed
anti-TNFα inhibitors (Key Patents: US App 08/446,674 / 20030064070A1; US
App 20020136723A1; US App 20020010180A1) for all indications reached
US$24.4 billion in 201114, most of which was used for the
treatment of rheumatoid arthritis. Interest in the therapeutic use of
biologics has blossomed since their discovery, with monoclonal antibodies
making up around one-third of drugs in the sector, essentially all for
chronic disease. High unit production costs of monoclonal antibodies are
falling as their use grows. New products are now also being launched,
including generic versions of the top selling antibodies as they lose
patent protection, which should eventually benefit patients and society.
It is predicted that by 2014, three of the four top drugs sold worldwide
will be anti-TNFs15, while the top 5 will be biologics,
monoclonal antibodies and antibody like fusion proteins. This shows the
outstanding impact of this research on the field of therapeutics15.
Sources to corroborate the impact
- Lichtenstein, G. R., Bala, M., Han, C., DeWoody, K. & Schaible, T.
Infliximab improves quality of life in patients with Crohn's disease. Inflamm
Bowel Dis 8, 237-243 (2002) DOI:
10.1097/00054725-200207000-00001 Paper reporting the impacts of
anti-TNFα therapy on the quality of life of patients with Crohn's
disease.
- van der Kooij, S.M. et al.Drug-free remission, functioning and
radiographic damage after 4 years of response-driven treatment in
patients with recent-onset rheumatoid arthritis. Ann Rheum Dis.
68:914-21 (2009). doi:10.1136/ard.2008.092254 Paper
reporting evidence that TNF treatment during early disease can
result in drug-free remission.
- National Institute for Health and Clinical Excellence. Rheumatoid
arthritis — etanercept and infliximab (NICE technology appraisal
guidance TA36) issued 2002.
http://guidance.nice.org.uk/TA36
[Accessed 2013] Original guidance endorsing the use of TNFα
inhibitors in rheumatoid arthritis. This guidance has been
superseded by Reference 11.
- Taylor, P.C., Feldmann, M. Anti-TNF biologic agents: still the therapy
of choice for rheumatoid arthritis. Nat Rev Rheumatol 5:578-82
(2009). doi:10.1038/nrrheum.2009.181 Review reporting that the
combination of an anti-TNFα agent with methotrexate remains the
therapy of choice to reduce the signs and symptoms of rheumatoid
arthritis.
- National Institute for Health and Clinical Excellence. [Guidance on
TNF inhibitors in RA (TA130, TA186, TA195) issued 2007 and 2010] http://guidance.nice.org.uk/TA/WaveR/61
Current NICE technology appraisal guidance outlining the optimal
use of biologics, and disease modifying antirheumatic drugs, for the
management of rheumatoid arthritis.
- British Society for Rheumatology and British Health Professionals in
Rheumatology guideline for the management of rheumatoid arthritis (after
the first 2 years) (2009) http://www.rheumatology.org.uk/includes/documents/cm_docs/2009/m/management_of_rh
eumatoid_arthritis_first_2_years.pdf. Updated clinical
guidelines outlining the optimal use of biologics, and disease
modifying antirheumatic drugs, for the management of rheumatoid
arthritis.
- Smolen J.S. et al. EULAR recommendations for the management of
rheumatoid arthritis with synthetic and biological disease-modifying
antirheumatic drugs. Ann Rheum Dis 69(6):964-975 (2010).
doi: 10.1136/ard.2009.126532 Clinical guidelines for the
management of rheumatoid arthritis, which recognise the importance
of the early introduction of biologic TNFα inhibitors for patients
failing to reach a treatment target of remission with DMARD drugs.
- R&D Pipeline News Apr 26 2012. Special Edn 1. Top 30 Biologics
2011.
http://www.pipelinereview.com/index.php/2012042647751/FREE-Reports/TOP-30-
Biologics-2011.html. (2013). Review outlining sales figures
and commercial outcomes of the research.
- Merck Research Laboratories. Slide from Senior Vice President, MRL
Franchise Head, Respiratory and Immunology. Email including data from
EvaluatePharma received 27th June 2012 (available on
request).