Improving treatment guidelines, life expectancy and access to life insurance for HIV positive people
Submitting Institution
University of BristolUnit of Assessment
Public Health, Health Services and Primary CareSummary Impact Type
HealthResearch Subject Area(s)
Medical and Health Sciences: Public Health and Health Services
Summary of the impact
In 2011, 34 million people worldwide were living with, and 1.7 million
died from, HIV/AIDS. Since 2002, HIV-positive people have benefited from
research by the Antiretroviral Therapy Cohort Collaboration (ART-CC) based
at University of Bristol (UoB). Research on the timing of ART led to
updated international HIV treatment guidelines that recommended starting
treatment earlier. Research on life expectancy highlighted the benefits to
patients of earlier ART, and was used by policy makers, clinicians and
patient groups to promote earlier treatment. Patients are now starting
treatment earlier resulting in increased life expectancy. Insurance
companies changed their criteria for providing life insurance, influenced
by ART-CC.
Underpinning research
2.1 The Antiretroviral Therapy (ART) Cohort Collaboration
ART-CC is a large collaboration set up in 2000 to study the survival of
HIV positive individuals starting treatment with ART. Funded by four
successive grants from the Medical Research Council, it includes nineteen
cohorts from Europe and North America and is coordinated by a team based
in the SSCM, UoB, led by Professor Jonathan Sterne and Dr Margaret May.
2.2 Informing treatment strategies
Analyses published in The Lancet in 2002, based on over 12000
patients, identified that the most important predictor of mortality was
the CD4 count, a measure of immune deficiency, at which patients started
ART [1]. Estimates of cumulative mortality for 80 risk groups were made
available via a web-based calculator (www.art-cohort-collaboration.org).
Scale-up of treatment in low-income countries started in 2002, and in 2006
ART-CC published the first comparison of mortality of patients starting
ART between low and high-income countries [2]. When patients and
physicians consider starting ART, they must balance its beneficial effects
in preventing AIDS and death with harmful side-effects and the
inconvenience of taking lifelong medication. Before 2009 the CD4 count at
which ART should be started was a central, unresolved issue in the care of
HIV positive people. ART-CC provided evidence that 350 cells/mm3
should be the minimum CD4 count below which ART should be started [3].
2.3 Life expectancy and the consequences of late treatment
ART-CC found that improvements in treatment for HIV decreased mortality
by nearly 40% and increased life expectancy by 13 years in high-income
countries between 1996-2005 [4], but that starting treatment too late
resulted in poorer survival [1,4]. May worked with the UK Collaborative
HIV Cohort (UK CHIC) Study to raise awareness amongst the general public
that starting treatment later than guidelines recommended resulted in up
to 15 years' loss of life [5]. For patients treated in the UK between 1996
and 2008, life expectancy was 13 years less than that of the UK general
population, and lower the later in the course of HIV disease that patients
started treatment. Life expectancy at age 20 was 38 years in those who
started ART with CD4 count <100, but >53 years in those who started
with CD4 between 200 and 350 cells/mm3.
2.4 Insurability of people living with HIV
In 2009, access to life insurance was very limited for people living with
HIV. Swiss Re (a reinsurance company based in Zurich, Switzerland)
collaborated with ART-CC to analyse data in the manner most useful for
promoting insurance by estimating excess mortality in HIV positive people
compared with expected mortality in the insured populations in 6 European
countries based on actuarial tables. This research showed that up to 50%
of HIV patients in lower risk groups could be eligible for life insurance
with terms up to 25 years [6].
ART-CC Co-ordinating Centre, University of Bristol team members
Prof Matthias Egger (2000-4 (Visiting Prof from 2004)); Prof Jonathan
Sterne (2000-present); Dr Margaret May (2000-present); Ross Harris
(2004-8); Dr Suzanne Ingle (2010-present).
References to the research
[1] Egger M, May M, Sterne JAC. et al. Prognosis of
HIV-1-infected patients starting highly active antiretroviral therapy: a
collaborative analysis of prospective studies. The Lancet. 2002 Jul;360
(9327):119 - 129. doi:10.1016/S0140-6736(02)09411-4
[2] Braitstein, P, et al (including May, Sterne, Egger).
Mortality of HIV-1-infected patients in the first year of antiretroviral
therapy: Comparison between low-income and high-income countries. Lancet,
2006. 367 (9513): p. 817-24. PMID: 16530575
doi:10.1016/S0140-6736(06)68337-2
[3] Sterne JA, May M, Costagliola D, Egger M et al.
Timing of initiation of antiretroviral therapy in AIDS-free HIV-1-infected
patients: a collaborative analysis of 18 HIV cohort studies. Lancet. 2009;
373 (9672): 1352-1363. PMID: 19361855 doi:10.1016/S0140-6736(09)60612-7
[4] ART-CC (including May, Sterne). Life expectancy of
individuals on combination antiretroviral therapy in high-income
countries: a collaborative analysis of 14 cohort studies. Lancet. 2008;
372 (9635): 293-299. PMID: 18657708 doi:10.1016/S0140-6736(08)61113-7
[5] May M, Gompels M, Delpech V et al. Impact of late diagnosis
and treatment on life expectancy in people with HIV-1: UK Collaborative
HIV Cohort (UK CHIC) Study. BMJ 2011, 343:d6016 doi: http://dx.doi.org/10.1136/bmj.d6016
[6] Kaulich-Bartz J, Dam W, May MT, Lederberger B et al. Sterne
JAC.Insurability of HIV-positive people treated with antiretroviral
therapy in Europe: collaborative analysis of HIV cohort studies. AIDS
2013; 27:1641-1655 PMID: 3678894 doi: 10.1097/QAD.0b013e3283601199
Medical Research Council (MRC) Peer Reviewed Grants
Sterne JAC (PI), Ingle SM, May M, Egger M, et al. Prognosis of
HIV-positive patients treated with antiretroviral therapy: comparative
analyses and treatment strategies. MR/J002380/1 £589,409 2012-15.
Sterne JAC (PI), May M, Egger M. et al. Monitoring and modelling
prognosis in the era of HAART. G0100221 £171,227, 2005-8 and G0700820
£627,188 2008-11.
Egger M (PI), Sterne JAC, et al. The impact of highly active
antiretroviral therapy: Monitoring and modelling benefit and potential
harm. G0100221, £218,046, 2002-5.
Details of the impact
4.1 Updated treatment guidelines resulted in earlier treatment
Earlier ART leads to better treatment outcomes for people with HIV
throughout the world with fewer deaths and hospitalisations. ART-CC's
research on prognosis [1-3] has been extensively cited by treatment
guidelines between 2008 and 2013. Our 2009 paper on timing of ART [3],
which clarified that the CD4 threshold for starting ART should be at least
350 cells/mm3, was particularly influential and informed
changes during 2009-11 to World Health Organization (WHO) [a], British
[b], European, US [c], and other national [d] guidelines to recommend
starting treatment earlier.
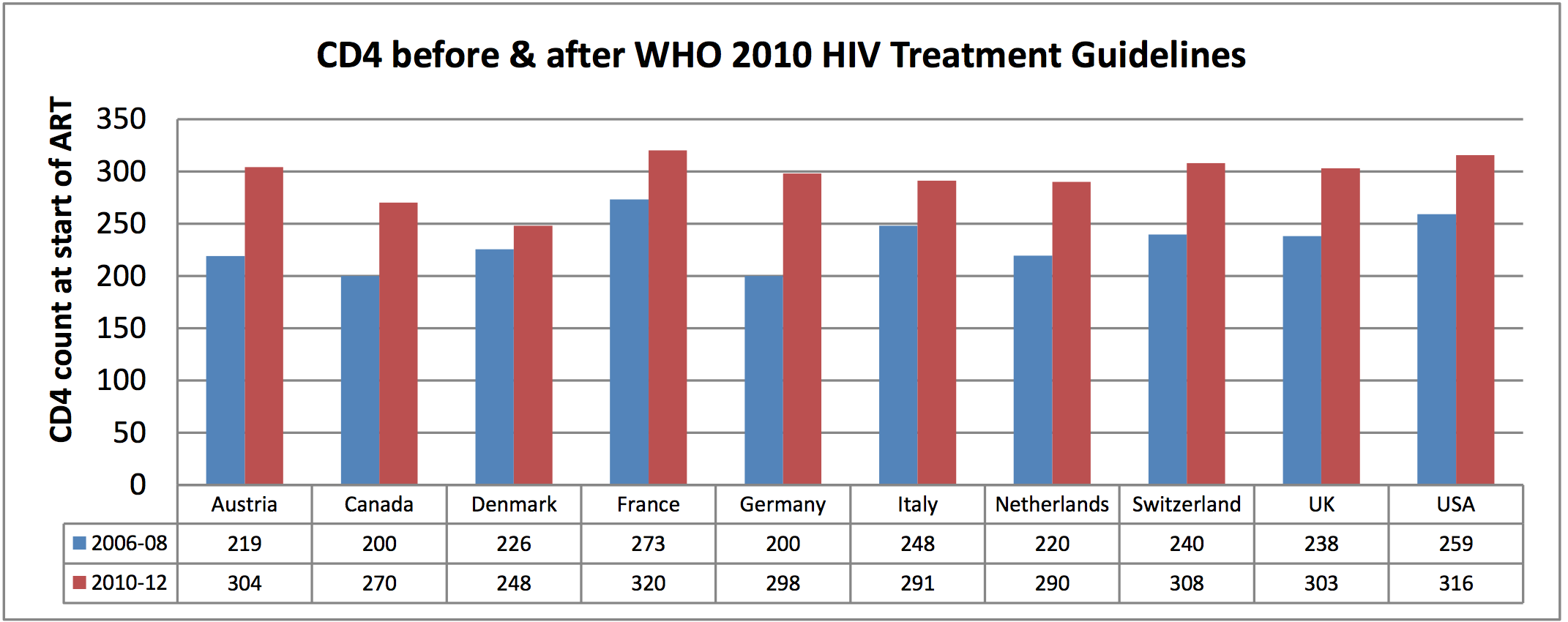
High income countries: ART-CC research suggests that increasing
the CD4 count at start of ART from 200 to 350 cells/mm3 will
increase life expectancy of a 20-year-old by between 8 [6] and 12 years
[5]. The bar chart on page 2 (based on unpublished ART-CC data) shows that
patients started treatment earlier in the UK, Europe and North America
after guidelines were changed in 2009-10. The Health Protection Agency
(HPA) 2012 report stated that between 2010 and 2011 AIDS diagnoses in the
UK decreased by 33% and mortality by 18% [e].
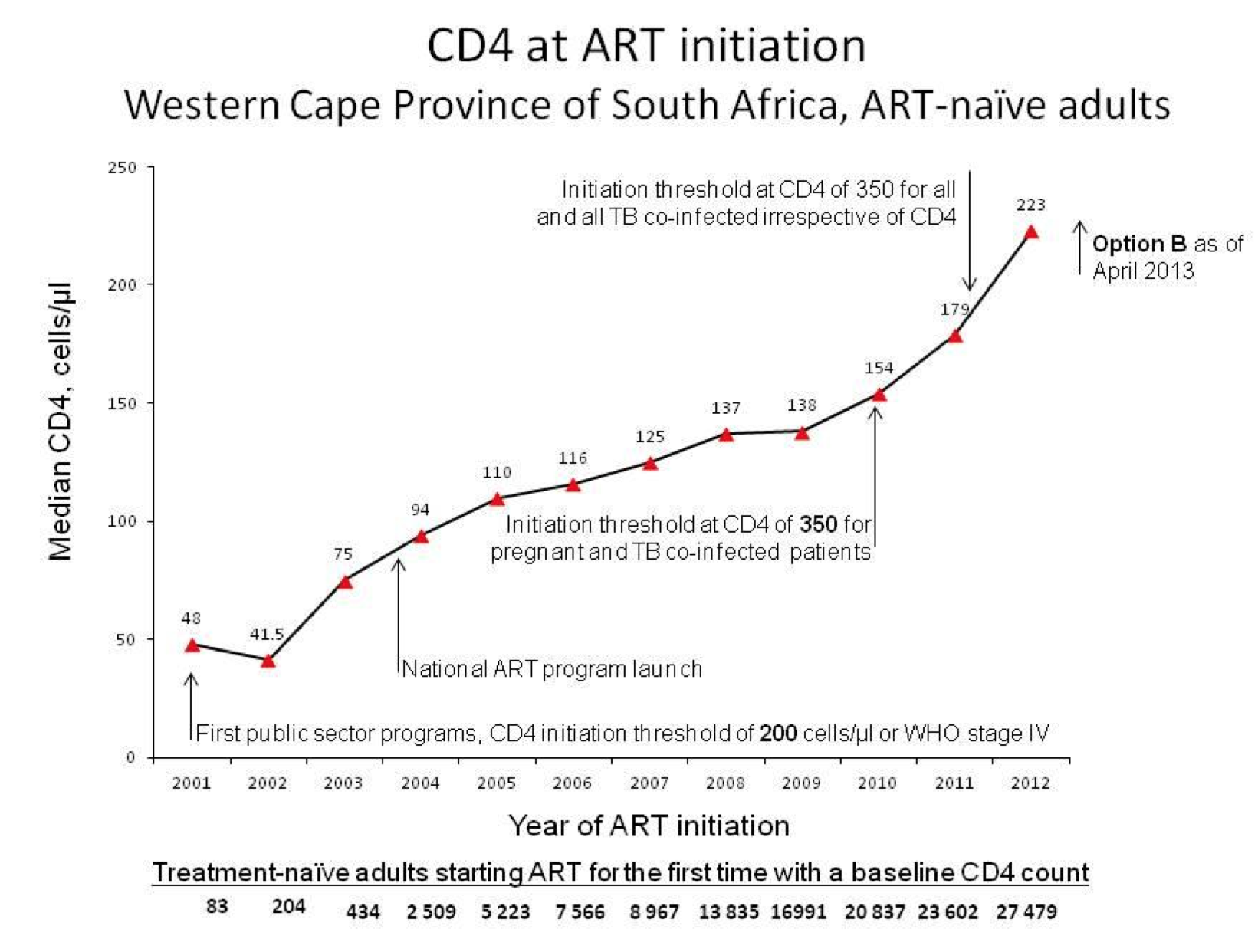
Low income countries: UNAIDS reported that the number of people in
Africa receiving ART increased from less than a million in 2005 to 7.1
million in 2012, with nearly 1 million added in 2012 alone. During 2009-11
the recommended threshold for treatment in at least 29 low and middle
income countries changed (based in part on ART-CC's work) from 200 to 350
cells/mm3 [d]. This has led to more and earlier treatment,
particularly in Africa. Data from Western Cape, South Africa, show the
steep increase in numbers of people treated and their increased CD4 count
at start of ART as a consequence of the adoption of the new guidelines
(graph — personal communication, Cape Town University, South Africa).
During this period, AIDS-related deaths in Africa fell by 32% from
approximately 1.75 to 1.19 million (calculated from UNAIDS 2012 global
report). The massive scale-up in treatment due to increasing the threshold
from 200 to 350 cells/mm3 has been replicated across the globe.
4.3 Raised public awareness of consequences of starting treatment late
May worked with the UK Collaborative HIV Cohort (UK CHIC) Study to raise
awareness of the loss in life expectancy due to starting HIV treatment
later than guidelines recommend [6]. This work was extensively reported in
the UK and worldwide, for example in a two-page feature in The
Independent in October 2011 [f] and in The China Daily [f]
and was also discussed by professional publications such as Nursing
Times, on 8 November 2011 [f]. The same research was presented in a
poster [f] displayed in hospital waiting rooms across the UK, to
communicate the findings to patients as part of a wider effort by UKCHIC
to disseminate information to key patient communities. According to the
2012 HPA UK HIV report, the proportion of HIV positive people diagnosed
late (with CD4 count below 350 cells/mm3) fell by 3% during
2011 [e].
The ART-CC paper on life expectancy [4] influenced a campaign to halve
the proportion of people diagnosed late with HIV [g]. The UK CHIC life
expectancy paper [5] contributed evidence to "Standard 1: HIV Testing and
Diagnosis" in the policy document from BHIVA on "Standards of Care for
People Living with HIV" [h]. Earlier diagnosis and prompt treatment
reduces onward transmission since successfully treated people with
suppressed virus replication do not transmit HIV [h]. This not only avoids
illnesses and early deaths, but also has the potential to deliver huge
financial savings. The HPA 2011 report estimated that the prevention of
one new HIV infection saves the public purse between £280,000 and £360,000
in direct lifetime healthcare costs [e]. This research therefore impacts
not only the 22,600 people the HPA estimated were living with undiagnosed
HIV in the UK in 2011 (2012 report) [e] but also uninfected individuals,
who are less likely to be exposed to HIV if those infected with HIV are
diagnosed and treated [e].
4.4 Improved access to insurance.
The opportunity to obtain life insurance has a major impact on quality of
life, particularly since a term of 20 years is required for a mortgage.
ART-CC research [1,6] had a commercial impact by providing data to
insurance companies that led them to improve the provision of life
insurance and open up the insurance market to HIV positive people. Swiss
Re [i], Hannover Re (UK) and AERAS (France) [i] based their assessment of
insurability of HIV positive people on ART-CC's publications [1,6] and
web-based mortality risk calculator. Based on our 2002 data [1], SwissRe
recommended that certain patient groups should be offered up to 10 years'
insurance. During 2010-12, ART-CC worked with SwissRe to extend this to 20
years and estimate the excess premium that HIV positive individuals would
need to pay [6]. This had an impact prior to publication: ART-CC tables
were presented at a national meeting of insurers in Paris [i], and New
York [i] by Swiss Re, and to the French AIDS research agency (Agence
Nationale de Recherche sur la Sida et les hepatites virales, ANRS) by
May[i]. Based on this research, Swiss Re updated its underwriting
guidelines for western Europe resulting in cheaper insurance costs and
broader coverage with policies offered up to 25 years [j]. The Head of
Research Innovation and Product Development, Swiss Re, stated that there
would be "greater access to home ownership and to business loans for HIV
positive persons" and the research "has led to increased normalisation of
HIV compared to other chronic diseases... The study has also influenced
Swiss Re's ratings for HIV+ lives in South Africa and the ratings of
direct insurers" and "has influenced debate on HIV ratings in India and
Australia" [j].
ART-CC research on insurability [6] has impacted awareness of insurance
products among HIV positive people through the work of advocacy groups
such as HIV i-base [i] and the European AIDS Treatment Group, which in
discussing our paper [6] wrote "People doing well on HIV therapy should be
eligible for life insurance" [i]. The proportion of UK insurers that
provide services to HIV positive people increased from 33% to 66% between
2010 and 2012 [i]. A 2012 UK survey found that the percentage of HIV
positive people who knew of the existence of life insurance products
increased from only 20% in 2012 to 78% in 2013 [i].
Sources to corroborate the impact
[a-d] corroborate influence of ART-CC research on changes in treatment
guidelines worldwide, [e-g] on earlier treatment, decreased AIDS and
deaths in UK, and [i-j] document increased provision of insurance based on
ART-CC analyses.
[a] WHO ART for HIV infection in adults and adolescents: recommendations
for a public health approach 2010 revision [cites 2 P65 & 3 P26] http://www.who.int/hiv/pub/arv/adult2010/en/index.html
[b] British HIV Association guidelines for the treatment of
HIV-1-positive adults with ART 2012 [cites 3 P22 and 5 P8] http://www.bhiva.org/documents/Guidelines/Treatment/2012/hiv1029_2.pdf
[c] US 2011: Guidelines for the use of antiretroviral agents in
HIV-1-infected adults and adolescents. 1/2011; 1-166. [cites 1 P7 &
extensively discusses 3 P28-9], revision 10/2011 [cites 4 P25] http://aidsinfo.nih.gov/guidelines
[d] Table of low and middle income countries that have changed guidelines
to start ART at CD4 count threshold of 350 derived from http://www.aidstar-one.com/
[e] HPA: HIV in the United Kingdom: 2011 [cites 5 P4] and 2012 Annual
Reports
http://www.hpa.org.uk/webc/HPAwebFile/HPAweb_C/1317131685847
and C/1317137200016
[f] Media, NHS and charities awareness reports after publication of paper
on life expectancy [5].
[g] Early testing saves lives: HIV is a public health priority. 2nd
edition Halve It Coalition.
http://www.bhiva.org/documents/Publications/Halve_it_Position_Paper.pdf
[cites 4 P7]
[h] BHIVA Standards of Care for People Living with HIV in 2013 - Standard
1: HIV Testing and Diagnosis [cites 5 P12] http://www.bhiva.org/standards-of-care-2012.aspx
[i] PDF Evidence of impact of ART-CC on insurability and awareness of
life insurance for HIV+.
[j] Personal statement: Director, Swiss Re.