Assessment and treatment of children and adults with face processing impairments
Submitting Institution
Bournemouth UniversityUnit of Assessment
Psychology, Psychiatry and NeuroscienceSummary Impact Type
HealthResearch Subject Area(s)
Psychology and Cognitive Sciences: Psychology
Summary of the impact
Prosopagnosia, or the inability to recognise faces, affects one person in
50, but public and professional awareness of the condition is low.
Bournemouth University (BU) established The Centre for Face Processing
Disorders (CFPD) to provide cognitive screening and training programmes to
improve recognition skills for affected adults and children. The centre
has grown significantly and, having tested over 100 people for
prosopagnosia, now treats 30 adults and 10 children through cognitive
training and clinical treatment. While patient numbers are moderate to
date, the service is unique in the UK and has provided proof of concept
for a scalable prosopagnosia diagnosis and a treatment approach. This
includes protocols for different conditions including Autism and Moebius
syndrome. In addition, the CFPD has orchestrated policy changes within
significant health organisations and charities.
Underpinning research
Less than six years ago, the incidence of face processing deficits was
thought to be very low. Parris (BU 2008-date) initially in collaboration
with colleagues at the University of Exeter, including Bate (BU 2010-date)
showed face recognition skills vary substantially within the normal adult
population (P1), and variation in childhood is also common. Genuine "face
blindness" (prosopagnosia) was, however, believed to be extremely rare.
Recent developments in research— combined with the easy availability of
information on the internet—have led to dramatic increases in estimated
incidence. It is now believed that the developmental form of prosopagnosia
affects up to one person in 50 worldwide. Some children with the condition
can encounter severe social and educational difficulties, demonstrating an
urgent need for a specific developmental screening assessment and
appropriate special needs provision. Likewise, adult sufferers who avoid
embarrassment through self-imposed social isolation may need specialised
psychological intervention.
BU acted swiftly to ensure the research programme could develop rapidly.
The Centre for Face Processing Disorders (CFPD) was established, with an
initial investment of £100k. Subsequently, Bate has led a prosopagnosia
research programme that underpins the clinical impact of the CFPD. For
example:
- Bate demonstrated that intranasal inhalation of oxytocin produces a
temporary improvement in face recognition skills in adults with
developmental prosopagnosia. This implies that the neural structures
that the hormone acts upon are open to modulation, even in prosopagnosia
(P4).
- The CFPD has developed a series of diagnostic tests using eye-tracking
software, which assess the visuo-cognitive processing strategies that
individuals with prosopagnosia typically employ. This work shows that
alternative physiological and behavioural measures can provide
bio-behavioural markers of face processing impairments, and highlights
the utility of more ecologically valid measures of face processing
skills (P2).
- In collaboration with Poole Hospital neurophysiologist Cole, CFPD has
obtained the first evidence that Moebius syndrome — a hereditary form of
facial paralysis accompanied by eye movement paralysis — can also result
in face recognition impairments. This corroborates previous findings
from unimpaired participants that eye movements are essential for face
recognition (P3).
References to the research
P1. Bate, S., Parris, B., Haslam, C. and Kay, J. (2010).
Socio-emotional functioning and face processing in the normal population.
Personality and Individual Differences, 48, 239-242. DOI
10.1016/j.paid.2009.10.005.
P2. Bate, S. and Cook, S. (2012). Covert recognition relies on
affective valence in developmental prosopagnosia: Evidence from the skin
conductance response. Neuropsychology, 26, 670-674.
DOI: 10.1037/a0029443.
P3. Bate, S., Cook, S.J. and Cole, J. (2013). First report of
generalized face processing difficulties in Möbius sequence. PLos One,
8(4), e62656. DOI: 10.1371/journal.pone.0062656.
P4. Bate, S., Cook, S.J., Duchaine, B., Tree, J.J., Burns, E.J.
and Hodgson, T.L. (2013). Intranasal inhalation of oxytocin improves face
processing in developmental prosopagnosia. Cortex, pii:
S0010-9452(13)00208-6 (e-pub ahead of print). doi:
10.1016/j.cortex.2013.08.006.
Details of the impact
Researchers at the CFPD have addressed the lack of awareness of
prosopagnosia through extensive dissemination of their research findings.
Significant impacts include developing diagnosis methods, cognitive
training and clinical treatment programmes to help prosopagnosia
sufferers. More recently the research has led to policy changes within
health organisations and charities. These interventions improve the lives
of sufferers, while demonstrating a proof of concept for a scalable
prosopagnosia diagnosis and a treatment approach.
Raising awareness
From the outset CFPD's research success depended on recruiting and
testing as many adults and children with prosopagnosia as possible. The
team set about raising awareness of the condition and the research, whilst
directing people to the website for recruitment and preliminary testing
(R1). They achieved this through media coverage, which significantly
increased public awareness of the condition. This is evidenced by the
sharp increase in visitor numbers to the website following key media
activity. This is shown in Figure 1, which also illustrates the
international reach of CFPD's work. Specifically in the last three years
the CFPD's work has featured on BBC South, CBBC, The Guardian,
Independent, Telegraph, Daily Mail, Mirror, Sun and Metro
among others.
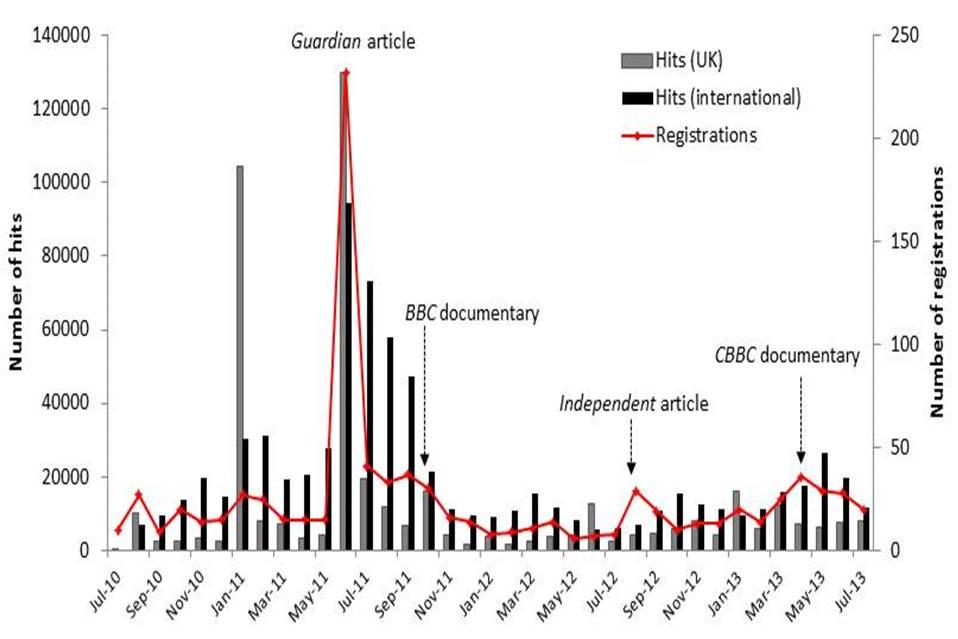 Figure 1: Page impressions and registrations on www.prosopagnosiaresearch.org
by month.
Figure 1: Page impressions and registrations on www.prosopagnosiaresearch.org
by month.
Media coverage of the CFPD is highlighted at relevant time points.
Source: Google keywords
Assessment and diagnosis
This strong, positive media interest, particularly following the formal
launch of CFPD in 2012, produced a step change in self-referral rate of
potential participants. This is evidenced by the fact that more than 900
people with face processing difficulties have now registered on the
website, compared with only 50 (40 adults and 10 children) in the 2 years
prior to the launch. All registrants are offered a cognitive screening
session that establishes whether they meet diagnostic criteria for
prosopagnosia. Face processing impairments are evident in other disorders
such as Moebius syndrome and Autism so the CFPD team has developed
protocols for differential diagnosis and tested over 100 individuals to
date.
CFPD maintains research links with laboratories in the USA (Dartmouth
College) and Australia (Centre of Cognitive Disorders: Macquarie
University and University of Western Australia), and regularly puts
international registrants in touch with these facilities, which also
provide diagnostic services.
The provision of prosopagnosia assessment is currently unique to the UK
and the availability of this service—even on a limited scale—has been
highly beneficial to individuals and their families. Frequently, they
report a sense of relief when long-standing difficulties in normal social
interaction are finally understood (R2).
Treatment
The significance of CFPD's work is in the development and evaluation of
research-based programmes for identifying and treating prosopagnosia.
These innovations can produce profound improvements in the quality of life
of people affected by the disorder.
The CFPD now has more than 30 adults and 10 children enrolled in
cognitive training programmes. Participants are typically required to make
fine-grained discriminations between pairs of similar faces. The task
becomes increasingly difficult as participants progress through levels in
a computer-game format, over a 12-week period.
Researchers are now investigating the effectiveness of combining these
programmes with oxytocin inhalation (P4) after demonstrating a temporary
improvement in face recognition skills following treatment with the
hormone. This is the first example of clinical intervention in the
treatment of prosopagnosia.
This proof of concept for a scalable assessment and intervention
programme has considerable reach, capable of serving the needs of the
estimated 300,000 children with prosopagnosia in the UK alone.
Organisational policy change
The CFPD's research, extensive dissemination and lobbying activities have
led to significant policy changes within health organisations and
charities.
NHS: Following dialogue with Bate, NHS Choices have committed to
have prosopagnosia added to the A-Z of conditions (R3). This was confirmed
in the House of Commons by Minister of State for Care and Support, Norman
Lamb MP on 02/07/2013, who said: "NHS Choices will be including
information about prosopagnosia in the A to Z of medical conditions on its
website later this year. This will help to promote better understanding
among the wider general public and ensure that people with prosopagnosia
receive the recognition and support they need" (R4).
In addition, Annette Brookes MP assisted in the formulation of an Early
Day Motion in Parliament to increase understanding of prosopagnosia as a
significant cognitive disorder (R5).
The Encephalitis Society The society provides support, awareness and
research for the inflammation of the brain. CFPD worked with the
organisation to produce a fact sheet about prosopagnosia. BU's contribution
can be confirmed through their Development Manager (R6).
Headway: CFPD researchers have worked with the brain injury
association Headway, to produce a fact sheet about how to cope with
prosopagnosia. This can be downloaded from Headway's site and BU's input
verified through their Information Officer (R7). In addition Headway have
added Bate's book Face Recognition and its Disorders to its Amazon
shop (R8).
Future applications
CFPD is continuing to expand the range of applications of its work. For
example, the techniques Bate has developed for improving face recognition
in prosopagnosia may also have value in extending the recognition skills
in unimpaired individuals. CFPD are currently working with the Scientific
Investigation Unit of the Dorset Police Force (R9) and Dorset Search and
Rescue (R10) to investigate the potential of this approach to create
`super-recognisers.' The Home Office has also asked CFPD to keep them
informed of their findings.
In summary, research by the CFPD has made significant strides in raising
awareness, assessing and treating individuals with face processing
disorders. The cognitive training programmes, combined with clinical
treatment with oxytocin, improve the lives of sufferers. The research has
led to important recognition of the disorder by the NHS and other
organisations. It is hoped BU's proof of concept for a scalable
prosopagnosia diagnosis and a treatment approach will help many more
sufferers in the future.
Sources to corroborate the impact
R1. Media coverage: www.prosopagnosiaresearch.org/media
R2. Participant testimonials: www.prosopagnosiaresearch.org/about/participant-testimonials
R3. NHS Choices: http://www.nhs.uk/Pages/HomePage.aspx
R4.Committment by Norman Lamb MP
http://www.publications.parliament.uk//pa/cm201314/cmhansrd/cm130701/text/130701w0004.htm#1307021000450
R5. Early Day Motion: http://www.parliament.uk/edm/2013-14/207
R6. CEO of the Encephalitis Society. Contact details available.
R7. Information Officer at Headway. Contact details available.
R8. https://astore.amazon.co.uk/headwathebrai-21
R9. Head of the Police Force's Technical and Forensic
Investigations Unit. Contact details available.
R10. Secretary of Dorset Search and Rescue. Contact details
available.
R11. Discussion board: www.prosopagnosiaresearch.org/discussion-board.