Facilitating positive cultural change in health and social care organisations through practice development
Submitting Institution
Bournemouth UniversityUnit of Assessment
Allied Health Professions, Dentistry, Nursing and PharmacySummary Impact Type
HealthResearch Subject Area(s)
Medical and Health Sciences: Public Health and Health Services
Summary of the impact
Bournemouth University (BU) has facilitated improvements to health and
social care practice
through cultural change in care provision. Researchers developed a
practice development
framework for implementing and assessing the delivery of evidence-based
practice in 82 UK health
and social care units during the impact period. Benefits to staff include
better communication and
team structure. Benefits to patients include higher standards of
cleanliness, privacy and dignity, as
well as a decrease in length of hospital stays and appointment waiting
times. Delivery has
extended to cover entire NHS Trusts serving a resident population of over
3.5 million, social
services departments and third sector organisations across the south of
England and beyond. The
research has since been applied to develop a similar system in Australia.
Underpinning research
The term `practice development' evolved from the work of a small number
of nursing development
units (NDU's) in England during the 1990's. Those in the South of England
were facilitated by BU.
The aim, based on research by Graham (BU 1994-2007), was to reduce the
theory-practice gap,
increase use of evidence-based practice, develop a better educated
workforce and move away
from the traditional medical model towards more patient-focused care.
After recognition at the time that this agenda could only be achieved
through multi-disciplinary
working, there was a shift from nursing-specific development to the wider
concept of inter-professional
practice development. BU researchers Warr (BU 2011 to present), McSherry
(BU
2008-2008), Graham and Keen (BU 2004 to present), focused on practice
development
approaches that would work across a wide variety of health and social care
settings (P1&2),
including NHS Trusts, social services departments and other organisations.
The research group identified a need for teams to question and challenge
current practice and, by
using evidence, improve services. The following research themes emerged,
which form the basis
of the standards of the Practice Development Units (PDUs) BU went on to
establish:
- Practice development is intended to improve person-focused care.
- Practice development should be practitioner owned and should empower
practitioners to
instigate change.
- To be effective practice development needs to bring about cultural
change.
- Practice development improves practice through the systematic
introduction of evidence-
based care.
From this, they established an explicit set of standards to measure the
quality of units against,
allowing successful departments to gain PDU accreditation or status.
Specific information on these
measures and the accreditation process is detailed in the impact section
of this case study.
More recently, researchers Todres (BU 1996 to present), Galvin (BU
1995-2012), Holloway (BU
2011 to present) and Hewitt-Taylor (BU 2002 to present) have examined the
practice development
approach in a wide variety of settings, such as specialist dementia (P6)
and children's (P4)
services. The department's current research into `humanisation' theory is
now being integrated into
the process to further enhance the quality of fundamental care offered to
service users (Francis
Report 2009, 2013). Humanisation of care is based on the principle that
restoring humanly
sensitive care is about how the `humanising focus' is clearly articulated
and kept alive as a primary
focus, next to other relevant targets. This theory has emerged from
pioneering research and
philosophical work undertaken by BU (P3).
Practice development is a continuous process of culture change and
service improvement through
enabling teams to transform the culture and context of care (Francis
Report 2009, 2013). It is
supported by facilitators committed to a systematic, rigorous and
continuous process of
emancipatory change.
References to the research
Publications
P1. McSherry, R. and Warr, J. (2008). An introduction to
excellence in practice development in
health and social care. Open University Press Maidenhead Berkshire
UK. ISBN: 978-0335223213.
P2. Fielding, C., Rooke, D., Graham, I. and Keen, S. (2008).
Reflections on a virtual practice
development unit: changing practice through identity development. Journal
of Clinical Nursing,
17(10), 1312-1319. DOI: 10.1111/j.1365-2702.2007.02043.x.
P3. Todres, L., Galvin, K. and Holloway, I. (2009). The
humanization of healthcare: a value
framework for qualitative research. International Journal of
Qualitative Studies on Health and Well-
being, 4(2), 68-77. DOI: 10.1080/17482620802646204.
P4. Hewitt-Taylor, J. (2012). Innovation in education for health
care assistants: a case study of a
programme related to children with complex and continuing health needs. Innovations
in Education
and Teaching International, 49(2), 99-110. DOI:
10.1080/14703297.2012.677597.
P5. Grant, A., Biley, F.C., Leigh-Phippard, H. and Walker, H.
(2012). The practice development
context. Journal of Psychiatric & Mental Health Nursing,
19(10), 950-957. DOI: 10.1111/j.1365-2850.2012.01921.x
P6. Hean, S., Nojeed, N. and Warr, J. (2011). Developing an
integrated memory assessment and
support service for people with dementia. Journal of Psychiatric &
Mental Health Nursing, 18(1),
81-88. DOI: 10.1111/j.1365-2850.2010.01665.x.
Grants
G1. 2008: Directly commissioned to undertake Practice Development
Accreditation for new
Children Centre Teams x 4 (a case study for the Department of Health) -
£31,000. PI: Andrews, C.
G2. Each practice development unit has been funded by their NHS or
Local Authority organisation
- £7,500. This amounts to over half a million pounds in total. PI:
Andrews, C.
G3. 2009: Five Rivers KTP Research Council Funded - £180,000,
Technology Strategy Board. PI:
Andrews, C.
G4. 2010: Help & Care KTP Research Council Funded - £192,556,
Technology Strategy Board.
PI: Hean, S.
Details of the impact
BU's practice development approach is now widely used in England (R1)
with further evidence of
use in Australia (R2). This helps health and social care practitioners to
use the best available
evidence to develop their practice and ensure their care is effective and
person focused.Through
the practice development process and accreditation teams work towards
developing a culture of
excellence by becoming person-centred and introducing evidence-based
practice through
effective culture change and teamwork. Teams are encouraged to question
and challenge current
practice and, by using evidence, improve services. Each PDU must
demonstrate:
- An understanding of the service user needs and clear mechanisms for
communicating and
listening to users and carers.
- How developments are researched, evidence-based, evaluated and
disseminated to
demonstrate best practice and to contribute to the local, national and
international
evidence base.
- A clear action plan that outlines the aims for development of services
and team members
that has links to national and local host organisation's priorities.
- A leadership structure that supports the delivery and development of
multi-agency inter-
professional care in line with the action plan.
- A defined communication structure to ensure the collaboration of team
members and the
provision of effective inter-professional care.
- A clear understanding of the user journey and understanding of the team
member's
contribution to the success of the user experience.
- How services have been developed taking a `whole systems' approach,
ensuring the entire
user journey is improved.
- Clear partnerships with an academic department and other agencies
required to support
research and the dissemination of best practice.
This explicit set of standards is then assessed by a panel of external
experts from practice and
academia who examine a portfolio of evidence and visit the unit to observe
and speak to service
users, carers and staff. Units are reaccredited on a three-yearly basis to
ensure high standards are
maintained.
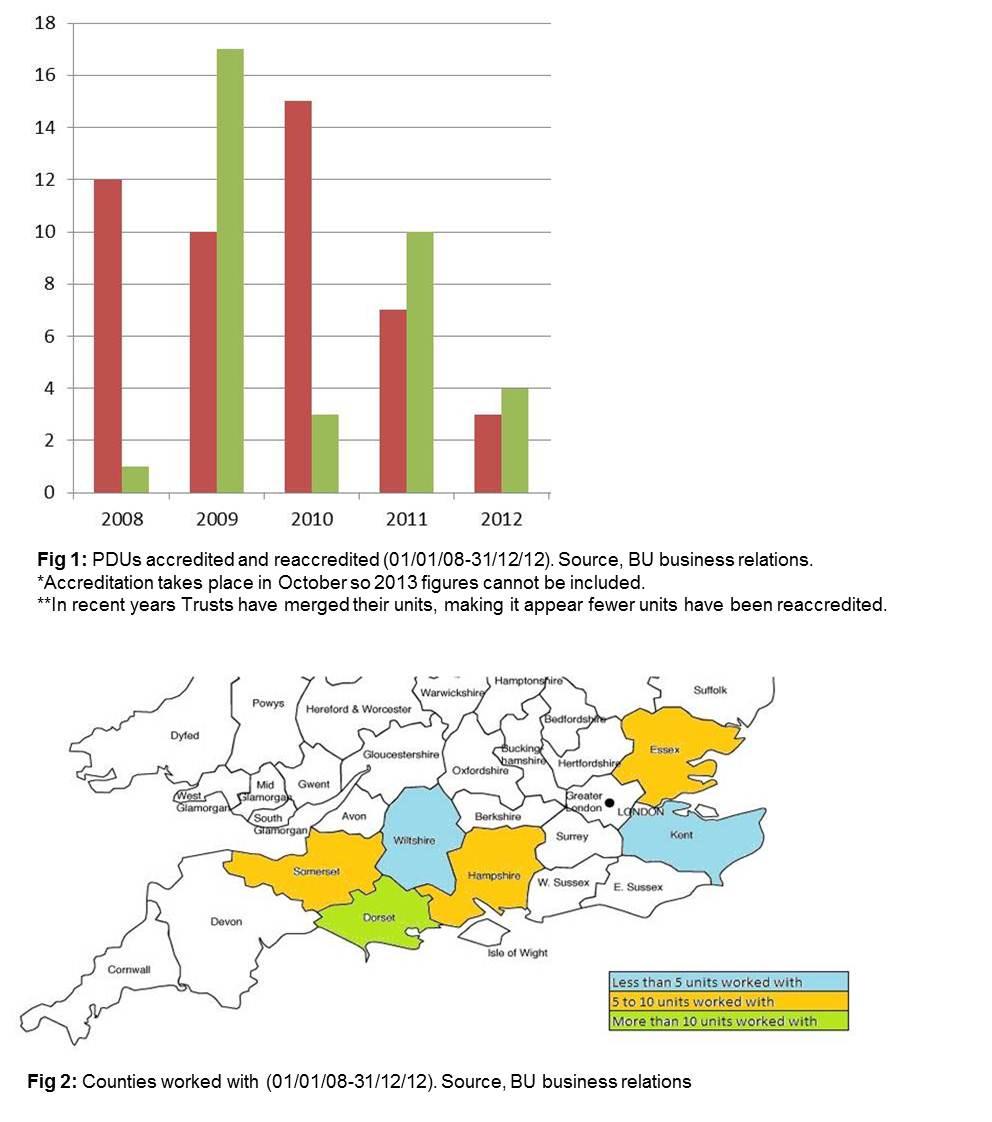
Since 2008, BU researchers have facilitated the set-up and accreditation
of 47 PDUs and
reaccreditation of 35 (Fig. 1), working with 82 units in total. This
covers 6 counties in the UK (Fig.
2), including 8 NHS Trusts serving a resident population of over 3.5
million (R3). Units accredited
and reaccredited include social services departments, dementia services
and children's units (R4).
The overarching impact of BU's practice development process is a change
in culture, leadership
and team creation. There is an extensive list of NHS and social care unit
contacts that can
corroborate this, demonstrating an effective move to evidence-based
practice, improved
communication between staff and service users and consistently improved
inter-agency working.
These include the following testimonials:
"Developments through practice development include pioneering work in
helping young people
with chronic conditions make the difficult transition from children's to
adult services; making
improvements to cleanliness; working with the public and patients to
revise visiting times and
protect patient privacy and dignity; introducing matron ward rounds and
reducing waiting times for
echo-cardiograms." Cardiology Department Matron — Poole Hospital NHS
Foundation Trust
(R5).
"Implementation of a new pain pathway through practice development after
total knee replacement
led to reduced pain and 0.5 day reduction in length of stay." Orthopaedic
Unit Ward Manager,
Poole Hospital NHS Foundation Trust (R6).
Organisations reap the benefits of multi-disciplinary teams and a
multi-agency approach, as well as
new leadership roles. Some further specific and measurable impacts
include:
- The North Essex NHS Foundation Trust `Patient Pathway', introduced
through BU's
practice development process in February 2010. This was achieved by
establishing working
groups who introduced training, amended recruitment criteria and
implemented essence of
care benchmarking for communication skills and continence management. One
year later,
there was an overall change in occupancy days since the pathway was
introduced. In one
ward the bed days reduced by 599 days overall, a 50 % reduction in length
of stay of
patients. This in turn reduces waiting lists and increases cost effective
for the NHS.
- The PDU at Poole Hospital NHS Foundation Trust led to streamlined
allergy testing in
2011, through the simplification of referral and appointment cancellation
mechanisms. This
resulted in appointment waiting times reduced from 13 weeks to 2 weeks.
Other reported benefits of practice development include a reduction in
pain through pain
management pathways, improvements to cleanliness, more patient-friendly
visiting times and
protection of patient privacy and dignity. Benefits on practice include
better communication
between staff and carers, a reduction in `inappropriate admissions', more
effective team
organisation and increased funding from service commissioners.
These benefits make a significant difference to treatment of patients and
working lives of staff in
Trusts serving a collective resident population of over 3.5 million. The
changes are also
contributing to a wider cultural change, which is necessary to improve
care. The continuing impact
of this research is evident through the development of PDU master classes
in Australia, formed
from the basis of BU programmes (R2).
Sources to corroborate the impact
R1. Crisp, J. and Wilson, V. (2011). How do facilitators of PD
gain expertise to support
transformation of practice and workplace culture? Nurse Education in
Practice, 11(3), 173-178.
DOI: 10.1016/j.nepr.2010.08.005.
R2. Hardy, S., Bolster, D., Kelly, T. and Yalden, J. (2012).
Enhancing facilitation skills through a
practice development masterclass. Australian Journal of Advanced
Nursing, 29(2), 36-47.
Available from: http://www.ajan.com.au/Vol29/29-2_Hardy.pdf
[accessed 21 November 2013].
R3. Sources for each NHS Trust sizes available on request.
R4. Statistics for Figures 1 and 2 available on request.
R5. Cardiology Department Matron, Poole Hospital NHS Foundation
Trust.
R6. Orthopaedic Unit Ward Manager, Poole Hospital NHS Foundation
Trust.
R7. Gallagher, J. and Fuggle, K. (2012). The Ideal way to
rejuvenate our service. Journal of
Dementia Care, 20(3), 14-15.
R8. Fitzgerald, A. (2008). Dementia Project One of UK`s Best. Maldon
& Burnham Essex
Chronicle.
R9. North Essex NHS Foundation Trust (2010). PDU Plaque Ceremony
Triumph, Crystal Centre
Newsletter, Essex County Council.
R10. Deep South Media (2012). Dorset Care Homes Celebrate
Badge of Excellence. Colten Care
Press Release.
R11. Dr Ann Hemingway: part of award winning public health PDU
team winning the DOH Health
and Social Care Award 2009 for partnership working on improving the sexual
health of young
people.
R12. Elson, J. (2010). Accreditation is the culmination of staff`s
efforts to improve services and
ultimately the standards of care that we provide. Director for Older
Peoples Services Dorset
Healthcare NHS Foundation Trust. The Beacon, Spring, 11.
R13. Fuggle, K. and Gallagher, J. (2012). Redesigning dementia
care through Practice
Development Accreditation (HR Manager and Operations Manager Colten Care
Nursing Homes).
The Beacon, Summer, 12-13.