HEAL03 - Promotion and support of breastfeeding for new-born infants
Submitting Institution
University of YorkUnit of Assessment
Public Health, Health Services and Primary CareSummary Impact Type
SocietalResearch Subject Area(s)
Medical and Health Sciences: Nursing, Paediatrics and Reproductive Medicine, Public Health and Health Services
Summary of the impact
Our research, which identified effective and cost-effective interventions
to help women, particularly those in low income groups, make informed
choices and establish and maintain breastfeeding for newborn infants, has
changed health policy and practice nationally and internationally. The
findings have been included in national and international practice
recommendations including National Institute for Health and Care
Excellence guidelines. Active dissemination of our research outputs and
adoption of their recommendations have been associated with stepwise
increases in breastfeeding rates in the UK, particularly for socially
disadvantaged women who typically have low breastfeeding rates, and is
likely to be associated with improved health of infants.
Underpinning research
Breastfeeding improves important outcomes for mothers and infants.
Initiation and maintenance of breastfeeding in the UK have historically
been low, particularly in socially disadvantaged young women.
Breastfeeding is particularly important for the 10% of infants born
preterm or with low birth weight (LBW). York researchers conducted seminal
systematic reviews which identified effective and cost-effective
interventions to increase rates of initiation and maintenance of
breastfeeding.
(i) Initiation of breastfeeding: Our systematic review of 59
studies evaluating a range of policy, supportive and educational
interventions showed the effectiveness of multi-faceted packages of
interventions including: targeted, small group, interactive education
programmes and peer support for women with low incomes (1). Our Cochrane
review of randomised controlled trials (RCTs) identified the substantial
benefits of interactive health education interventions. For every 100
women receiving education, 20 extra initiated breastfeeding (2).
(ii) Maintenance of breastfeeding: Our Cochrane review of 34 RCTs
involving ~30000 mother-infant pairs in 14 countries showed that extra
support for women (particularly integrated lay and professional support)
increased the duration of breastfeeding. For every 100 women receiving
extra support, 5 more continued to breastfeed up to six months (3).
(iii) Breastfeeding infants in neonatal units: Our systematic
review of the effectiveness of interventions to promote breastfeeding or
feeding with expressed breast milk for infants admitted to neonatal units
(4) included 8 studies from 17 countries. We reported strong evidence for
the effectiveness of parent-baby "skin-to-skin" contact and UNICEF Baby
Friendly Initiative (BFI) accreditation. Our cost-effectiveness analysis
found that enhanced contact and support reduced overall costs and
increased "quality adjusted life years" for preterm or LBW infants,
especially those with very low birth weight (5). Our Cochrane review found
that feeding preterm or LBW infants in response to hunger and satiation
cues rather than a caregiver-led regimen shortened both transition to oral
feeding and hospital stay (6).
Researchers: Britton (Lecturer, Nov 1996 - present); Craig
(Research fellow, Nov 2004 - present); Dyson (Research fellow, Feb 2005 -
present); Lister-Sharp (Research fellow June 1996 - June 2002); McCormick
(Research fellow, Nov 2004 - Dec 2012); McFadden (Research fellow, Nov
2004 - Dec 2012); McGuire (Professor, Dec 2008 - present); O'Meara
(Research fellow, Nov 1995 - June 2013); Renfrew (Professor, Nov 2004 -
July 2012); Rice (Research fellow, Mar 2003 - present); Sowden (Senior
Researcher, Feb 1994 - present).
References to the research
1. Fairbank (Dyson) L, O'Meara S, Renfrew MJ, Woolridge M, Sowden AJ,
Lister-Sharp D. Systematic review to evaluate the effectiveness of
interventions to promote the uptake of breastfeeding. Health Technol
Assess 2000;4(25):1-171. DOI: 10.3310/hta4250
2. Dyson L, McCormick FM, Renfrew MJ. Interventions for promoting the
initiation of breastfeeding. Cochrane Database Syst Rev
2005;(2):CD001688. DOI: 10.1002/14651858.CD001688
3. Britton C, McCormick FM, Renfrew MJ, Wade A, King SE. Support for
breastfeeding mothers. Cochrane Database Syst Rev
2007;(1):CD001141 DOI: 10.1002/14651858.CD001141.pub3 [updated 2012]. DOI:
10.1002/14651858.CD001141.pub4
4. Renfrew MJ, Craig D, Dyson L, McCormick F, Rice S, King SE, et al.
Breastfeeding promotion for infants in neonatal units: a systematic review
and economic analysis. Health Technol Assess 2009;13(40):1-146.
DOI: 10.3310/hta13400
5. Rice SJ, Craig D, McCormick F, Renfrew MJ, Williams AF. Economic
evaluation of enhanced staff contact for the promotion of breastfeeding
for low birth weight infants. Int J Technol Assess Health Care
2010;26:133-40. DOI: 10.1017/S0266462310000115
6. McCormick FM, Tosh K, McGuire W. Ad libitum or demand/semi-demand
feeding versus scheduled interval feeding for preterm infants. Cochrane
Database Syst Rev 2010;(2):CD005255. DOI:
10.1002/14651858.CD005255.pub3.
This research was funded from the following competitive grants:
• Systematic review of factors which promote or inhibit the initiation of
breastfeeding. NHS R&D HTA programme. £56,000; 1998-9 (Lister-Sharp).
• Systematic review of interventions to promote the initiation of
breastfeeding. Canadian Child Health Field Bursary, Cochrane
Collaboration. £3304; 2002-3 (Dyson).
• NICE Public Health Collaborating Centre for Maternal and Child
Nutrition. £446,000; 2004-7 (Renfrew, Dyson).
• Infant feeding for babies in Special and Intensive Care Units. NIHR HTA
programme: £204,000; 2007-8 (Craig, Renfrew).
Details of the impact
Active dissemination of the research as a pathway to impact
We planned a targeted dissemination and implementation strategy to
promote the adoption of our research findings into practice in health
services across England. This included distribution of 60,000 copies of an
Effective Health Care bulletin (http://www.york.ac.uk/inst/crd/EHC/ehc62.pdf), which
summarised the findings of our systematic review of interventions to
promote the initiation of breastfeeding, to NHS practitioners and
service-users and supported this with a targeted media campaign. Second,
we produced a NICE `Evidence into Practice' briefing based on our
systematic reviews of interventions to promote breastfeeding. Finally we
conducted a national consultation with health professionals and
management, government, service user and voluntary organisations which
highlighted that the routine implementation of multifaceted, local
packages of breastfeeding services and the UNICEF UK BFI standards for
maternity services should be priorities for action (nice.org.uk/aboutnice/whoweare/aboutthehda/hdapublications/promotion_of_breastfeeding_initiati
on_and_duration_evidence_into_practice_briefing.jsp). Our
dissemination and implementation strategy has helped our research have a
significant impact on national and international health policy, clinical
guidelines, staff education, practice, and infant feeding behaviour as
outlined below.
Impact on policy statements, guidelines, toolkits and care pathways
Our work has directly contributed to the development of national and
international policy, including NICE Clinical Guidelines (CG) which UK
healthcare professionals are expected to follow.
--Initiation and maintenance of breastfeeding
- The NICE `Evidence into Practice' briefing which we produced was
referenced explicitly for its specific contribution to formulating
recommendations in the full NICE Clinical Guidance on postnatal care (in
2006 and updated in 2012) as well as being cited 16 times in the text.
This included the priority recommendation that all maternity care
providers in acute and primary settings should implement care using the
UNICEF UK BFI as a minimum standard (source 1).
- Our reviews and evidence summary documents were incorporated into the
NICE Maternal and Child Nutrition Public Health Guidance CG 037 (source
2) and the 2008 NICE CG on antenatal care (source 3). Both
NICE documents cited the reviews as evidence to support specific
recommendations for "interactive antenatal breastfeeding education" and
"one-to-one counselling and peer support", using the UK UNICEF BFI as a
minimum standard.
- The recent evidence document underpinning the 2013 revision of the UK
UNICEF BFI standards cited our reviews and evidence summary documents
more than 20 times (source 4).
- Our systematic reviews are cited in guidelines in Australia and the
USA:
- The Australian National Health & Medical Research Council
(NHMRC) Infant Feeding Guideline cites reference 3 in recommending
"evidence-based actions for promoting the initiation and duration of
exclusive breastfeeding" (source 5).
- The US Surgeon General's Call to Action to Support Breastfeeding
cites our research (refs 1 and 3) as the basis for recommending
"professional and lay support [.] to increase the duration of
breastfeeding", and for adoption of UNICEF-BFI training (source 6).
--Breastfeeding in neonatal units
- The systematic reviews of interventions to promote breast (milk)
feeding for infants in neonatal units (refs 4, 6) informed the
development of the NICE CG on donor breast milk banks (source 7),
the Department of Health toolkit for high-quality neonatal services (source
8), and the UNICEF-BFI guideline for neonatal units (source 9).
- The Australian NHMRC Infant Feeding Guideline cites ref 4 as providing
evidence that "expressed breast milk reduces the incidence of
necrotising enterocolitis" among preterm infants (source 5).
- WHO Guidelines on optimal feeding of LBW infants in low/middle-income
countries cites our review (ref 6) as evidence to recommend feeding
infants based on hunger cues (source 10).
Impact on education and training
Our work has had a direct influence on staff education and training. It
has formed the basis for the three modules on infant feeding of the
Department of Health-funded Royal College of Paediatrics and Child Health
e-learning programme on early years, freely available since 2009 to all
health professionals in the UK [www.rcpch.ac.uk/hcp].
Prof Renfrew worked closely with the charity "Best Beginnings" to produce
a DVD ('From Bump to Breastfeeding') www.bestbeginnings.org.uk/fbtb
which promotes and supports breastfeeding based on evidence from our
systematic reviews. 1.5million copies have been distributed free to
pregnant women throughout the UK since 2008.
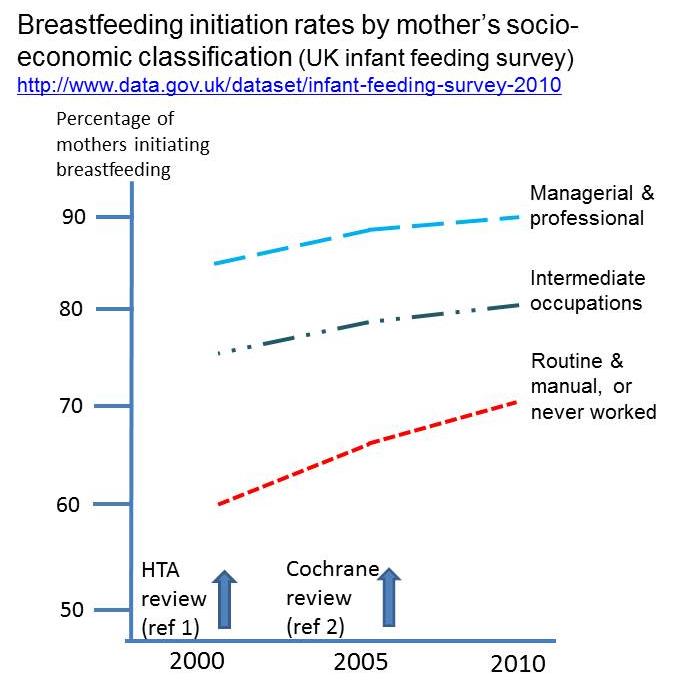
Impact on behaviour and outcomes
-- Initiation of breastfeeding
Data from the Infant Feeding Survey, collected every 5 years since 1990
and standardised for factors associated with breastfeeding (age, education
and social class), show that breastfeeding initiation remained static at
62% of all women in England & Wales between 1990 and 2000. Comparable
data in 2005 and 2010, however, show a 5% point increase at each time
point in the number of women starting to breastfeed since the start of the
York research programme, from 62% in 2000 to 72% in 2010 (source 11).
Standardised data are not available by socio-economic group, but non-
standardised data (see graph) indicate relatively larger and sustained
increases in the proportion of women from lower socio economic groups
starting to breastfeed in England & Wales from 2000 to 2010. This is
consistent with York's research (source 11). Changes in the
definitions used to categorize "socio-economic status" limit the direct
comparability of data from the IFS prior to 2000. However, no increases in
breastfeeding initiation rates were observed between 1995 and 2000 for
both "non-manual" (81%) and "manual" occupation households (61% ) before
this research was carried out.
-- Maintenance of breastfeeding
The 2010 UK Infant Feeding Survey found that the proportion of women
maintaining breast-feeding has continually increased from 2005. The
prevalence of breastfeeding at six weeks was static at 45% between 1995
and 2000, but then rose to 48% in 2005 and 55% in 2010. Six months rates
were 21% in both 1995 and 2000, but then rose to 25% in 2005 and 34% in
2010. Exclusive breast-feeding rates have also increased (at three months
they were 17% in 2010 compared with 13% in 2005, and at four months they
were 12% in 2010 compared with 7% in 2005). Rates of increase were highest
in low income women, reflecting our research recommendations to focus on
those where the potential to impact on important health outcomes is
greatest (source 11).
-- Health outcomes
Increased rates of breastfeeding, particularly amongst those at higher
risk improves health outcomes in infants in the short and long term. The
UNICEF report, Preventing
Disease and Saving Resources, estimates that even
moderate increases in breastfeeding could see millions in potential annual
savings to the NHS from improved health outcomes (source 12).
--Breastfeeding in neonatal units
In 2010, as part of the DH-funded regional Health Innovation and
Education Cluster (HIEC), York developed educational packages to support
quality-improvement initiatives to promote bonding, attachment and
breastfeeding in neonatal units based on our research. Following
implementation of recommendations from our reviews, the prevalence of
skin-to-skin care in neonatal units across Yorkshire & the Humber
increased from 20% in 2010 to >40% in 2012 and receipt of breast milk
on discharge from 40% to 52% (source 13). This has resulted in all
UK units now collecting breast (milk) feeding outcomes within the UK
national routine audit systems and the RCPCH National Neonatal Audit
Programme. This national audit found that the proportion of very preterm
infants receiving any breast milk at discharge rose from 54% in 2011 to
58% in 2012, which will reduce mortality and morbidity associated with
diseases such as necrotising enterocolitis (source 14).
Sources to corroborate the impact
- Routine postnatal care of women and their babies. NICE guideline
(2006) www.nice.org.uk/CG037
- Maternal and child nutrition: NICE public health guidance 11 (2008) www.nice.org.uk/PH11
- Routine care for the healthy pregnant woman. NICE guideline 62 (2008).
www.nice.org.uk/CG062
- Entwistle FM (2013) The evidence and rationale for the UNICEF UK
Baby Friendly Initiative standards. UNICEF UK.
- Infant Feeding Guidelines. National Health and Medical Research
Council (2012). www.nhmrc.gov.au/guidelines/publications/n56
- US Department of Health and Human Services. The Surgeon General's Call
to Action to Support Breastfeeding. Department of Health and Human
Services, Office of the Surgeon General (2011).
- Donor breast milk banks. NICE clinical guideline 93 (2010). www.nice.org.uk/CG093
- Department of Health. Commissioning local breastfeeding support
services (2009). http://webarchive.nationalarchives.gov.uk/20130107105354/http://www.dh.gov.uk/prod_consum_dh/groups/dh_digitalassets/documents/digitalasset/dh_106497.pdf
- Nyqvist KH et al. Expansion of the Baby-Friendly Hospital Initiative
ten steps to successful breast-feeding into neonatal intensive care:
expert group recommendations. J Hum Lact 2013;29:300-309. DOI:
10.1177/0890334413489775
- Guidelines on optimal feeding of low birth weight infants in low-and
middle-income countries. World Health Organization (2011). Available
from: www.who.int/maternal_child_adolescent/documents/infant_feeding_low_bw/en/
- McAndrew F, et al. Infant Feeding Survey 2010 www.esds.ac.uk/doc/7281/mrdoc/pdf/7281_ifs-uk-2010_report.pdf
- Preventing disease and saving resources: the potential of increasing
breastfeeding in the UK unicef.org.uk/Documents/Baby_Friendly/Research/Preventing_disease_saving_resources.pdf
- Yorkshire & Humber HIEC. Turning best practice into common
practice. Final report (2013) yhhiec.org.uk/wp-content/uploads/2013/07/12120503_HIEC_Report_2012_2013_PRINT-FINAL.pdf
- National Neonatal Audit Programme, Annual Report 2012. www.rcpch.ac.uk/system/files/protected/page/RCPCH_NNAP_Report%202012%20(2).pdf