Building and Implementing a Replicable Model for HIV Testing and Counselling
Submitting Institutions
University of Liverpool,
Liverpool School of Tropical MedicineUnit of Assessment
Clinical MedicineSummary Impact Type
PoliticalResearch Subject Area(s)
Medical and Health Sciences: Public Health and Health Services
Summary of the impact
Research at the Liverpool School of Tropical Medicine (LSTM) has
developed a successful approach to the rapid scale-up of HIV Testing and
Counselling (HTC) services in high prevalence countries, a vital component
of the global HIV response. The model combines comprehensive quality
assurance with operational research and has led to HTC expansion in
mobile, home and facility-based settings. It has also allowed for
responsiveness to local needs leading to post rape care services linked to
HTC, services for the deaf and HTC for men who have sex with men (MSM) and
other hidden populations in Africa. The global impact of this model is
reflected in WHO policy, Ministry of Health HTC guidelines in numerous
countries in Africa, the on-going work of an indigenous Kenyan NGO and
expansion of HTC through community outreach in the UK.
Underpinning research
Through a range of collaborations in Africa, Asia and the UK, LSTM has
led research in the development and scale-up of quality assured, complex
interventions to increase diagnosis of HIV, prevent transmission and
improve HIV outcomes especially in generalised HIV epidemic areas and
amongst adolescents and marginalised groups. LSTM staff who conducted this
body of research has included Charles Gilks (Prof 1995 - 2002), Gillian
Arthur (Clinical Lecturer 1999 - 2002), Miriam Taegtmeyer (Senior Clinical
Lecturer 2001 - present), seconded to Kenya in 2001 - 2004 where she
founded a local NGO, Liverpool Voluntary Counselling and Testing (LVCT),
David Lalloo (Dean of Clinical Sciences 1999 - present) and Sally Theobald
(Reader in Social Science 2001 - present).
HTC services using rapid diagnostic (20 minutes) HIV tests have helped
millions of people learn their HIV status, and for those testing positive,
learn about options for long term care and treatment. These rapid tests
are highly sensitive and specific, they can be performed with a
finger-prick blood sample; they do not require electricity or laboratory
machines and can be performed by a health care worker or trained lay
counsellor, making them suitable for use outside of health facilities.
Confirmation through a second rapid test can provide immediate and final
results, allowing onward referral and linkage to other services. LSTM
conducted a DfID-funded pilot project in 1999 assessing the feasibility,
acceptability and cost of integrating these newly available rapid tests
into three primary health centres in Kenya. Integration was found to be
both acceptable and feasible, to be associated with behaviour change and
significantly reduced cost. It represented a significant improvement on
previous practice where deferred results led to 47-66% of persons tested
not receiving results [1].
Research headed by Taegtmeyer during her time in LVCT, led to the first
published descriptions of translating these pilot studies into the
scale-up of HTC services in high prevalence countries, a vital component
of the global HIV response. Firstly describing expansion to 350 sites in
Kenya [2], and how this was accompanied by a robust quality assurance
system [3]. Additional operational research compared costs of mobile and
stand-alone HTC services provided to 62,173 clients [4], discussed human
resource implications and informed choices in mass media promotion for HTC
that underpinned policymaker decisions to diversify models for HTC in
Kenya from 2004 onwards as mobile services were found to be cost
effective, lay counsellors to provide accurate results through a task
shifting approach and media promotion that directly mentioned HIV positive
results to be more successful than that which did not. The demand of
services from vulnerable groups led to further studies on best approaches
to deliver HTC services for post-rape care [5], for the deaf [6] and for
men who have sex with men [7] in Africa as well as on improving linkages
to HIV care among newly diagnosed positives, for example through home
initiation of services.
Qualitative studies in the UK indicated acceptability and feasibility of
similar approaches to point of care testing for HTC, although impact data
was required before commissioners in the UK would make this part of
routine HIV services. LSTM therefore conducted a pilot study in 2009-2010
in Liverpool using similar training, community entry, supervisory methods
and radio interview outreach as done in Kenya. This brief 2009 pilot
resulted in 953 tests and 17 new positives diagnosed and linked to care
and treatment, an approach that is now funded by commissioners and
integrated at the Royal Liverpool University Hospital.
References to the research
Key Research Grants
2013-2014 (1 year). Bill and Melinda Gates Foundation.
Operational Characteristics of HIV self-test prototypes in lay users in
sub-Saharan Africa. $187,000. Miriam Taegtmeyer. (PI)
2013 - 2017 (4 years). FP7 Framework for Health. REACHOUT - close
to community services. €5.8 m. Miriam Taegtmeyer. (PI)
2010 - 2015 (5 years). CDC. Institutional collaboration between
LSTM and CDC and Prevention on Malaria and HIV. $1.8 m. Miriam
Taegtmeyer. (PI)
2001 - 2003 (2 years). DFID. VCT scale-up in government health
facilities in Kenya.. £320,000. Miriam Taegtmeyer (PI)
2012 - 2015 (3 years). Wellcome Trust. ES Postdoctoral Research
Fellowship - The social impact of HIV self-testing: reconstructing
knowledge and re-framing risks associated with HIV prevention. £443,455. David
G Lalloo & Robert Heyderman (PI's)
Details of the impact
HIV presents a significant health burden in Kenya with an estimated
104,000 infected children and 1,192,000 persons living with HIV infection
in 2012 [8]. Early treatment has been associated with a 96% reduction in
onwards transmission of HIV and theoretical modelling has shown that
testing scale-up accompanied by treatment could lead to the eradication of
HIV within a decade. LSTM's research has increased testing, both directly
through the changes in policy and systems in Kenya and indirectly through
the scalable quality assured services delivered in institutions like LVCT.
Health Impact
LVCT was founded by Dr Taegtmeyer to exploit the LSTM research findings
on best practice for the delivery of quality assured HTC. The finding
shaped the NGO's practice and is maintained today through methodologies
documented by Taegtmeyer and referenced within the Kenya National
Voluntary Counselling and Testing (VCT) guidelines in 2010 [9]. LVCT has
grown into an internationally acclaimed indigenous Kenyan organisation
(t/o US$ 9.2m pa). Dr. Kilonzo, Director of LVCT, completed her PhD at
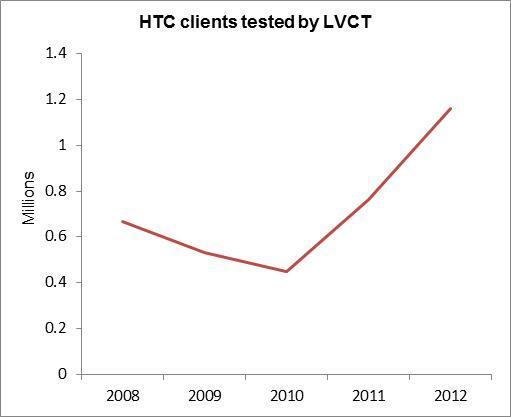
LSTM. LVCT continues to have a direct reach in HTC services in Kenya, as
shown in the graph and supports post rape care services in 84 health
facilities in 2012. The principles established in the early research have
enabled rapid scale-up including mobile, outreach and home-based testing.
A sound quality basis has facilitated adaptations to enable services for
the deaf and other vulnerable groups including MSM and post-rape cases.
The LVCT annual report [10] documents delivery of quality assured HIV and
counselling to 1,159,970 clients, with 223,645 children, couples, MSM,
persons with disabilities and sex workers in 2012. Levels of HIV testing
have increased with 72% of adults aged 15 to 64 years in 2012 reporting
ever having been tested for HIV, a significant increase from 34% in 2007.
HIV prevalence among adults aged 15 to 64 years decreased nationally from
7.2%, to 5.6% in 2012, as indicated in the Kenya AIDs Indicator Survey
[8].
The methodology documented by Taegtmeyer and LVCT was rolled out in 2008
onwards in other African countries and multiplied through WHO policies and
guidelines. Partner agencies include the Ministries of Health in Ethiopia
(focus on access to disadvantaged populations), Cote d'Ivoire (home
testing) and Botswana and Tanzania [11] (quality assurance). The 2012
CDC/WHO handbook for planning, implementing and monitoring home-based HTC
in high prevalence countries, was developed by Taegtmeyer and is globally
available [12].
Policy Impact
Kenya: Dr Taegtmeyer was part of the editorial team of the first
national guideline for VCT in Kenya. This was used as the basis for the
updated guidelines in 2007 and the later second edition in 2010 [9] with a
focus on provider initiated counselling and testing, quality improvement
systems and inclusion of the option for HIV self-testing. The guideline
changed practice and the approach to HTC with the establishment of a QA
taskforce that developed a QA strategy for HTC linked to the new
guidelines. The initial Kenyan quality assurance resource pack published
in 2003 has been the basis of the 2012 National Quality Management
Guidance Framework [13] for HIV testing and counselling in Kenya 2012.
International: LSTM research findings on HTC have gained
considerable attention of international policy makers and significantly
impacted policy on HTC in the WHO and at the US government's Centres for
Disease Control (CDC). Taegtmeyer was a member of the PEPFAR counselling
and testing team from 2007 - 2012. Taegtmeyer was the primary writer of
WHO's Handbook for Improving HIV Testing and Counselling Services,
published in 2010, translated into French and Mandarin [14]. Taegtmeyer
also led the writing of a Practical Handbook on Planning, Implementing and
Monitoring Home-based HTC [12], and was part of the core writing group of
the Operational and Service Delivery Guideline Development Group for the
WHO ART guidelines in 2013 [15]. Recommendations from the WHO on HIV
re-testing were published in 2010 in French and English [15] and
Taegtmeyer led on the expert consultation on acute HIV infection in
Atlanta which was the basis of these recommendations. LSTM initiated the
first ever international symposium on self-testing for HIV, Taegtmeyer and
Theobald contributed to the consensus statement agreed by UNAIDS, WHO, and
the Brocher Foundation in April 2013 [17, page 33], on the legal, ethical,
gender, human rights and public health implications of HIV self-testing
scale up. Special acknowledgements were made to Taegtmeyer in the meeting
report. [17, page 34]
UK: The research in 2009 led the Liverpool Centre for Sexual
Health to adopt point of care testing as a direct consequence of the pilot
and it is now in routine clinical use for HIV same day testing service,
(730 POCT in 2012) targeting at risk individuals and was presented in a
national forum that saw the beginning of the scale-up of point of care
services in a range of sexual health clinics in the UK [18].
Sources to corroborate the impact
Each source listed below provides evidence for the corresponding numbered
claim made in section 4 (details of the impact).
- Kenya AIDS Indicator Survey 2012, Preliminary Report,
http://nascop.or.ke/library/3d/Preliminary%20Report%20for%20Kenya%20AIDS%20indicator%20survey%202012.pdf
- National Guidelines for HIV Testing and Counselling in Kenya, 2nd
Edition, October 2010. http://nascop.or.ke/library/HTC/National%20Guidelines%20for%20HTC%20in%20Kenya%202010.pdf
- LVCT Annual Report 2011/12 http://www.lvct.org/images/pdf/annual%20report%202012-2013.pdf
- Tanzania Standard Operating Procedures for HIV Testing and counselling
services.
http://www.jica.go.jp/project/tanzania/001/materials/pdf/vct_10.pdf
- Home-based HIV counselling and testing: CDC and WHO Practical Handbook
for planning, implementing and monitoring home-based HTC in high
prevalence countries (2012)
http://www.cdc.gov/globalaids/Resources/prevention/docs/HomeBasedHIVTestingAndCounsellingHandbook.pdf
- National Quality Management Guidance Framework for HIV Testing and
Counselling in Kenya (2012)
http://nascop.or.ke/library/HTC/National%20QMG%20Framework%20Final.pdf
- WHO Handbook for improving HIV testing and counselling services Nov
2010. Taegtmeyer, LSTM first author http://www.who.int/hiv/pub/vct/9789241500463/en/index.html
- Consolidated guidelines on the use of antiretroviral drugs for
treating and preventing HIV infection (2013) http://www.who.int/hiv/pub/guidelines/arv2013/en/
- Delivering HIV results and messages for re-testing and counselling in
adults (2010) (French and English). http://whqlibdoc.who.int/publications/2010/9789241599115_eng.pdf
- Report with consensus statement, on the first international symposium
on self-testing for HIV April 2013. http://apps.who.int/iris/bitstream/10665/85267/1/9789241505628_eng.pdf
- Contact: Lead Nurse, Liverpool Centre for Sexual Health, Directorate
of Sexual Health & HIV Medicine, Royal Liverpool and Broadgreen
University Hospitals, can confirm numbers of Point of Care HIV same day
testing, now in routine clinical use since 2009.