Minimally invasive procedural training for clinicians using virtual patients
Submitting Institution
Bangor UniversityUnit of Assessment
Computer Science and InformaticsSummary Impact Type
HealthResearch Subject Area(s)
Physical Sciences: Other Physical Sciences
Information and Computing Sciences: Artificial Intelligence and Image Processing
Engineering: Biomedical Engineering
Summary of the impact
We demonstrate the impact of deploying real time 3D computer graphics and
haptics technologies
in the context of training minimally invasive procedures. It is widely
accepted in medical specialties
that a reform in teaching methods must be made to meet today's high volume
training
requirements. Receiving instruction in a core set of skills and procedures
before novice
practitioners are exposed to the traditional, patient based,
apprenticeship model has been shown
will reduce the time needed to acquire skills, maintain competence, and
reduce the initial errors
made on patients. The case study centres on three simulators developed at
Bangor (Figure 1).

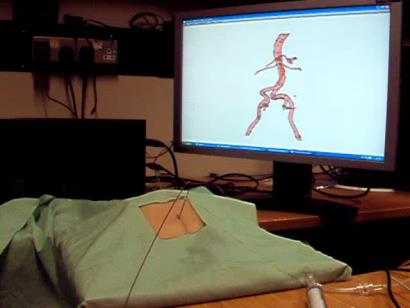
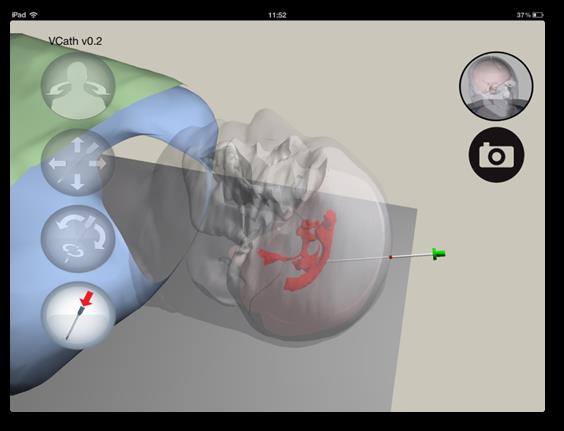 Figure 1: Minimally Invasive Procedural Training Simulators
Figure 1: Minimally Invasive Procedural Training Simulators
Underpinning research
Since 2003, Bangor School of Computer Science has led and coordinated
multi-disciplinary
research to build and deploy virtual patient systems for training
minimally invasive procedures. The
collaborations have involved computer scientists from Bangor, Imperial,
Leeds and Hull; clinicians
from Liverpool, Leeds and Cardiff, clinical engineers from Liverpool, and
psychologists from
Manchester. The research team from Bangor involved in this work are:
- Prof Nigel W. John, research management, implementation, coordination
and
commercialisation activities, 2003 — present
- Dr Franck Vidal, PhD Student (2003-8), Research Officer at Bangor,
2006-2008, appointed
as a lecturer at Bangor, 2011
- Dr Chris Hughes, Research Officer, 2006 - 2013
- Dr Serban Pop, Research Officer, 2007 — present
- Dr Llyr ap Cenydd, Research Officer, 2007 - 2013, appointed as a
lecturer at Bangor, 2013
- Prof Michael Rees, Consultant Cardiologist, School of Medical Sciences
and Betsi
Cadwaller University Health Board, 2005 — present
- Prof Derek Gould, Consultant Interventional Radiologist (Royal
Liverpool Hospital) and
Honorary Professor in Bangor School of Computer Science, 2006 — present
- Dr Tim Coles, PhD student, 2008-2011
A virtual patient is a sophisticated computer model of a human that can
deliver accurate real time
physiological responses to a trainee clinician using their natural senses
and skills. Variations in
patient anatomy and pathology, interaction between surgical tools and
tissues, and human
physiology such as respiration and blood flow must all be taken into
account. The main impact of
using virtual patients has been to reduce risk to real patients, reduce
clinical training costs, and
help clinicians maintain skills.
The Bangor team developed algorithms for haptic effects of a needle
penetration into tissue of the
virtual patient, generating ultrasound-like images from CT source data,
GPU implementations of X-Ray
and fluoroscopy image generation, and managed the integration of the
simulators. More
specifically we:
- Proposed a volume haptic model for simulating needle puncture into
different tissue types,
using patient specific (CT) data [3.1].
- Designed and built a novel hardware haptic needle holder interface and
simulation software
(Fig 1B) [3.2]. EPSRC (EP/E002587), award to Bangor (John PI): £342,005
(total grant:
£1,858,982). Patent pending [3.4]. This invention supports the
introduction and orientation
of a real needle into the virtual patient, assists with guiding the
needle, and includes a
pressure sensor to detect the position of the operator's finger tips.
- Developed a haptics simulation of a virtual ultrasound scanner that is
used to guide the
needle to the correct location inside the patient (Fig 1A) and utilises
GPU-accelerated
simulations of X-Ray transmission imaging [3.3]. Dept. of Health HTD
Programme, award to
Bangor (John PI): £108,051(total grant: £450,213).
- Produced the first prototype simulator to use augmented reality as a
training aid in
interventional radiology [3.5].
- Acquired data from actual procedures for use in and validation of
simulations. For example,
worked on optimisation of angioplasty by investigating the mechanism of
balloon
angioplasty and using intravascular imaging.
- Produced a novel tablet based training tool (VCath) for practicing a
neurosurgery procedure
on an iPad (Fig 1C).
- Have written well cited position papers on haptics in medical
simulation [3.6] and
intravascular imaging and measurement (Rees, 2011, 40 citations).
References to the research
1. F.P. Vidal, N.W. John, A.E.Healey, D.A. Gould,
"Simulation of Ultrasound Guided Needle
Puncture using Patient Specific Data with 3D Textures and Volume Haptics",
Computer
Animation and Virtual Worlds. Vol 19, Issue 2, pp111-127, 2008, Online
ISSN: 1546-427X,
Print ISSN: 1546-4261. DOI: 10.1002/cav.217
63 citations (Google Scholar November 2013). Returned in RAE 2008
2. V. Luboz, C.J. Hughes, D.A. Gould, N.W. John, F. Bello,
"Real-time Seldinger Technique
Simulation in Complex Vascular Models", International Journal of Computer
Assisted
Radiology and Surgery. Vol.4 No. 6, p 589-596. 2009. DOI:
10.1007/s11548-009-0376-0.
15 citations (Google Scholar November 2013) (submitted to REF2014 ID
1102).
3. P.F. Villard, F.P. Vidal, C.Hunt, F. Bello, N.W. John,
S. Johnson, D.A. Gould, "A Prototype
Percutaneous Transhepatic Cholangiography Training Simulator with
Real-time
Breathing Motion", International Journal of Computer Assisted Radiology
and Surgery.
Vol.4 No. 6, p 571-578. 2009. DOI: 10.1007/s11548-009-0367-1
17 citations (Google Scholar November 2013)
4. C. J. Hughes, N.W. John, "Haptic Needle as part of Medical
Training Simulator", EP
Patent 2,497,077, US Patent 20,120,219,937, 2011
5. T.R. Coles, N.W. John, D.A. Gould and D.G. Caldwell,
"Integrating Haptics with
Augmented Reality in a Femoral Palpation and Needle Insertion Training
Simulation"
IEEE Transactions on Haptics: Special Issue on Haptics in Medicine and
Clinical Skill
Acquisition, vol. 4., no. 3, pp 199-209, May-Jun 2011, DOI:
10.1109/TOH.2011.32
15 citations (Google Scholar November 2013) (submitted to REF2014 ID
1101).
6. T. R. Coles, D. Meglan, N. W. John, "The Role of
Haptics in Medical Training Simulators:
A Survey of the State of the Art". IEEE Transactions on Haptics, vol. 4,
no. 1, pp. 51-66,
Jan.-Mar. 2011, DOI:10.1109/TOH.2010.19
73 citations (Google Scholar November 2013) (submitted to REF2014 ID
1104).
(Authors in bold are from the Bangor team)
Details of the impact
As a result of the CRaIVE collaboration (5.6), two unique high fidelity
training simulators for
interventional radiology and cardiology procedures have been deployed, one
of which was
awarded a European Medical prize in 2009 for its "innovative use of
computer graphics in a
complex system that is already far advanced towards clinical use" (5.7).
Related work is on-going
to utilise mass market hardware such as tablet computers (5.10, 5.11). The
Bangor team have
taken the lead role in exploitation activities. Optimisation work carried
out on interventional
procedures such as angioplasty also provides unique data that can be
exploited in the next steps
of the training simulator after the catheter has been deployed. These
activities contributed directly
to a £1.2 million grant award in 2011 from the Wales Government that has
established an
Advanced Medical Imaging and Visualization unit (March 2011), led by John,
with a remit to work
in direct collaboration with the NHS delivering added value to everyday
practice in hospitals
through the use of visual computing technologies (5.3). The VCath App
(5.11) and an electric
wheelchair driving simulator (5.4) are two examples of simulation outputs
from the unit at Bangor.
The simulators provide an objective assessment of task performance and
the Bangor team
contributed to novel metrics that provide, arguably, the first
opportunities for validated proficiency
assessments in interventional radiology needle access. The simulators have
been rigorously
validated by our psychology collaborators (5.8, 5.9) after full ethical
approval was obtained. These
content, face and construct validity, and skills transfer studies show
that training on a virtual patient
does provide a demonstrable improvement of users' performance. In training
a simulated
percutaneous nephrostomy (an image guided needle puncture), results from
53 participants
showed that 78% of participants had indicated that the design was
realistic, with content validity
being rated averagely for all critical task steps; 83% of participants
found the simulator a useful
model for training skills for nephrostomy. In training the Seldinger
Technique, results from the 28
participants who completed the simulated procedure, lend support for the
simulator's face validity
(82% agrees the simulator would be effective for learning basic skills and
86% believes it would be
useful in learning how to use equipment). In addition, results from 26
radiology registrars who
completed four trials on the simulator, showed that on average,
participants' performance improved
on all metrics over four trials on all metrics used to assess performance.
The cost of hardware
components used in the this work is modest, totalling under £10,000 for
each high fidelity
simulator, including haptics interfaces, offering an affordable solution
to skills acquisition within a
credentialing organisation's curriculum, as well as for simulation
training centres and hospitals'
training programmes.
We have also been collaborating with neurosurgeons to produce a low
fidelity training application
for deployment on the iPad computer tablet platform (5.1, 5.2, 5.11). The
Bangor team have
implemented a tool for learning the ventricular catheterisation procedure,
which involves inserting a
cannula into the ventricles within the brain so that fluid can be drained.
The VCath App is the
world's first example of an interactive procedure training tool to be made
available on an iPad
using a virtual patient and a finger gesture interface. The App passed
Apple's quality assurance
checks at the first attempt and is available for free download on the
iTunes store. Over 6,500
downloads world-wide occurred since its launch in October 2012, and the
current average is over
400 downloads per month, demonstrating far reaching dissemination. Further
funding from
NISCHR has been awarded for a validation study of VCath. Many other
training tools for targeting
tasks such as for nephrolithotomy (removal of kidney stones) can be
similarly delivered and we are
leading the way forward in this area.
License agreements with companies operating in the surgical simulation
marketplace have been
discussed, and are on-going, e.g., an evaluation agreement is in place
with G-coder Systems AB
of Sweden who market surgical training interfaces (5.5). However, more
direct deployment in the
short term has been based on a public domain model. Advanced Practice
Courses using the
interventional simulators are being planned since the start of 2013 with
the indicated approval of
the British Society of Interventional Radiologists and road shows have
been organised in which the
training simulators are made available free of charge with support from
the Bangor team. The next
road show event will be held at Ysbyty Gwynedd in January 2014.
Sources to corroborate the impact
Neurosurgeon collaborators:
-
Liam Gray, Institute of Psychological Medicine and Clinical
Neurosciences, Cardiff
University, mailto:GrayWP@cardiff.ac.uk;
-
Nick Phillips, Leeds General Infirmary, mailto:Nick.Phillips@leedsth.nhs.uk.
- The Senior Project Manager at NISCHR can be contacted for
corroboration on Bangor's
leading role in the Advanced Medical Imaging and its impact on everyday
practice in
hospitals using visual computing technology.
- Clinical contacts to have benefitted include: the Clinical Director of
the North Wales Medical
Physics, Ysbyty Glan Clwyd Hospital, who can be contacted for
corroboration.
- The CEO of G-coder Systems AB, Sweden (http://www.g-coder.com)
can confirm interest
of using simulator software from Bangor in commercial domain.
- CRaIVE (Collaborators in Radiological Interventional Virtual
Environments) Network
http://www.craive.org.uk/
- Eurographics Medical prize (2009). Awarded second place for:
ImaGINe-S: Imaging Guided
Interventional Needle Simulation (Fig 1A).
http://www.eg.org/images/stories/awards/dirk_bartz_price/halloffame_20120525.pdf
- SJ Johnson, CM Hunt, HM Woolnough, M Crawshaw, C Kilkenny, DA Gould, A
England, A
Sinha, PF Villard. Virtual reality, ultrasound-guided liver biopsy
simulator: development and
performance discrimination. British Journal of Radiology. 85.1013
(2012): 555-561, DOI:
10.1259/bjr/47436030.
- SJ Johnson, SM Guediri, C Kilkenny, PJ Clough. Development and
validation of a virtual
reality simulator: human factors input to interventional radiology
training. Hum Factors.
(2011) Dec;53(6):612-25. http://www.ncbi.nlm.nih.gov/pubmed/22235524
- "How a brain surgery app could save lives", BBC News coverage on the
neurosurgery iPad
App training tool (VCath, Fig. 1C), January 2013 (http://www.bbc.co.uk/news/uk-wales-20948542).
- iTunes store download link: https://itunes.apple.com/sg/app/vcath/id568887198?mt=8