UOA01-22: FOXP1: Enabling Targeted Cancer Therapy
Submitting Institution
University of OxfordUnit of Assessment
Clinical MedicineSummary Impact Type
TechnologicalResearch Subject Area(s)
Medical and Health Sciences: Clinical Sciences, Oncology and Carcinogenesis
Summary of the impact
Researchers from the University of Oxford identified the novel human
protein Forkhead box transcription factor 1 (FOXP1) and showed it to be an
important prognostic biomarker in cancer. Expression of FOXP1 can
distinguish those patients with diffuse large B-cell lymphoma (DLBCL) who
are at high risk of disease progression, making it possible for clinicians
to target more intensive therapy to this group. DLBCL accounts for one
third of lymphomas and is the seventh commonest form of cancer. The
anti-FOXP1 monoclonal antibody developed by Oxford University is now used
worldwide in clinical diagnostics.
Underpinning research
In 1999 Professor Alison Banham's group at the University of Oxford
Leukaemia Research Fund Immunodiagnostics Unit identified the novel human
FOXP1 transcription factor, as well as a subfamily of related FOXP
transcription factors, and was the first to patent the use of FOXP1 as a
potential biomarker. FOXP1 is responsible for regulating gene expression
during normal development and adulthood; however, dysregulated FOXP1 can
lead to haematological malignancies, including diffuse large B-cell
lymphoma (DLBCL) and solid tumours. Increased expression of FOXP1 in DLBCL
with a post-germinal centre (or activated B-cell) phenotype was linked to
poor survival (patent: PCT/GB00/04590) and identified FOXP1 as a potential
tumour suppressor protein(1). The University of Oxford
researchers then developed JC12, the first anti-FOXP1 specific monoclonal
antibody. The development of the JC12 antibody was a major advance in this
field, making it possible for clinicians to measure the FOXP1 protein in
patients' cells, using relatively straightforward and direct
immunocytochemistry labelling techniques.
In 2003 an international collaborative study instigated by Professor
Banham showed that FOXP1 expression predicted DLBCL with a high-risk of
progression2. This was independent of the International
Prognostic Index (the conventional clinical scoring system used to predict
outcome)2. In 2009, a further collaboration with the highly
influential Lymphoma/Leukemia Molecular Profiling Project, run by the US
National Institutes of Health, confirmed the importance of FOXP1 protein
expression in identifying the clinically relevant molecular subtypes of
DLBCL. Significantly, this study also showed high FOXP1 expression in
DLBCL patients with the more aggressive activated B-cell subtype disease3.
Researchers from the University of Oxford have also played a pivotal part
in highlighting the potential for FOXP1 as a biomarker in prostate and
breast cancer. Collaborations between Professor Banham and Professor
Adrian Harris at the Weatherall Institute of Molecular Medicine,
University of Oxford, using the JC12 antibody, showed the significant
correlation of FOXP1 expression with oestrogen receptors and survival4,5.
FOXP1 was found not to be oestrogen regulated5, suggesting that
FOXP1 and oestrogen receptors may share a common regulatory pathway.
In 2007, Oxford researchers were the first in the world to report smaller
isoforms of FOXP1 associated with a more aggressive activated B-cell
subtype of DLBCL6. The existence of these potentially oncogenic
smaller isoforms represents a possible answer to the contradictory
findings that FOXP1 represents a favourable prognostic marker in breast
and prostate carcinomas, while also representing an adverse risk factor in
B-cell lymphomas.
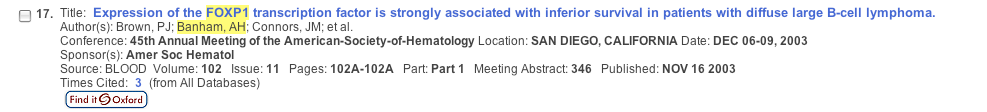
References to the research
2. Banham AH, et al. Expression of the FOXP1 transcription factor is
strongly associated with inferior survival in patients with diffuse
large B-cell lymphoma. Clin Cancer Res 11: 1065-72 (2005).
Available at
http://clincancerres.aacrjournals.org/content/11/3/1065.full.pdf+html(accessed 2013)
This paper presents the results of research originally presented in
the Abstract shown below with the same authors published in Blood
102A, Part 1, Meeting Abstract 346 thus providing evidence of a 2003
priority date.
3. Choi WW, et al. A new immunostain algorithm classifies diffuse large
B-cell lymphoma into molecular subtypes with high accuracy. Clin
Cancer Res 15: 5494-502 (2009). doi: 10.1158/1078-0432.CCR-09-0113
Available at http://clincancerres.aacrjournals.org/content/15/17/5494.long (accessed 2013)
The analysis of FOXP1 protein expression was identified
by the National Institute of Health Lymphoma/Leukemia Molecular
Profiling Project Group as being a vital component of a panel of
antibodies for classifying DLBCL and identifying high risk patients.
4. Fox SB, et al. Expression of the Forkhead transcription factor
FOXP1 is associated with estrogen receptor and improved survival in
primary human breast carcinomas. Clin Cancer Res 10: 3521-27
(2004). doi: 10.1158/1078-0432.CCR-03-0461 Available at
http://clincancerres.aacrjournals.org/content/10/10/3521.full.pdf+html (Accessed 2013)
Paper supporting a role for FOXP1 as a
possible co-regulator of the estrogen receptor in breast cancer and
also providing evidence for a role in the regulation of additional
pathways involved in cancer development.
5. Bates GJ, et al. Expression of the forkhead transcription factor
FOXP1 is associated with that of oestrogen receptor in primary invasive
breast carcinomas. Breast Cancer Res Treat 111: 453-459
(2008). doi 10.1007/s10549-007-9812-4
Available at http://link.springer.com/content/pdf/10.1007%2Fs10549-007-9812-4 (Accessed 2013)
This paper reported that FOXP1 expression correlated significantly
with oestrogen receptorb as well as oestrogen receptora and survival
in primary invasive breast cancer. Importantly FOXP1 expression was
not oestrogen regulated.
6. Brown PJ, et al. Potentially oncogenic B-cell activation-induced
smaller isoforms of FOXP1 are highly expressed in the activated B
cell-like subtype of DLBCL. Blood 111: 2816-2824
(2008) doi: 10.1182/blood-2007-09-115113
Available at
http://bloodjournal.hematologylibrary.org/content/111/5/2816.long (accessed 2013)
This paper provides the first description of the presence of smaller
isoforms of FOXP1 during normal B-cell activation and cell lines and
patient samples derived from activated B-cell DLBCL. It was suggested
that these smaller isoforms could represent a mechanism for increased
FOXP1 expression in this DLBCL subtype and that they might be
functionally distinct from the full length protein.
This research was funded by the Leukaemia and Lymphoma Research Fund,
Cancer Research UK, the Breast Cancer Campaign, Isis University Innovation
Fund, the Starmer Smith Memorial Fund, the Association of International
Cancer Research, and Tenovus.
Details of the impact
Diffuse Large B cell Lymphoma (DLBCL) is the most common
non-Hodgkin's lymphoma. It accounts for approximately a third of
lymphomas, and is the seventh most common cancer, with an annual incidence
of 25,000 cases in the USA. Despite recent improvements in therapies,
fewer than 50% of patients survive for more than 5 years.
Gene expression profiling has identified two different types of DLBCL,
the germinal centre-subtype and the more aggressive activated B-cell
derived subtype, which is associated with markedly inferior survival rates7.
Accurate identification of these DLBCL subtypes in patients allows more
specific targeted therapy, and will ultimately improve a patient's chance
of survival.
Although gene expression profiling had linked FOXP1 expression to the
activated B-cell DLBCL subtype (associated with inferior survival rates)8,
this technique was not found suitable for routine clinical use. This paved
the way for the accurate detection of FOXP1 using simple and reproducible
immunostaining methods.
Research performed at Oxford showed a good correlation between results
obtained from gene expression profiling and the use of antibody JC12 in
immunocytochemical staining9, leading to this methodology being
used in clinics worldwide for routine diagnostic procedures.
Major steps in achieving worldwide use of JC12 in routine diagnostics
include the following series of trials:
- A collaboration initiated by Professor Banham demonstrating that
immunolabelling with the monoclonal antibody JC12, identified patients
with poor prognosis activated B-cell subtype of DLBCL, under the new
gold standard treatment, CHOP-R10.
- Clinical collaborations between Professor Banham (Oxford) and the
French Groupe d'Etudes des Lymphomes de l'Adulte supported the clinical
relevance of FOXP1 expression in CHOP-R treated DLBCL, in two randomised
trials LNH98-5 and LNH01-5B11.
- The international CORAL study identified FOXP1 as being of prognostic
relevance for predicting progression free disease in DLBCL12.
- In 2012 the International DLBCL Rituximab-CHOP Consortium Program
Study recognised that FOXP1 expression was one of the three most
significant molecules for predicting outcome in DLBCL. Significantly,
they confirmed that the addition of a FOXP1 antibody to a panel of
antibodies used in routine immunostaining purposes constituted a highly
effective panel for defining clinically relevant DLBCL subtypes13.
The anti-FOXP1 monoclonal antibody, JC12, has since been licensed for
research and in vitro diagnostic use worldwide14. The
JC12 antibody is routinely used to classify DLBCL and to identify patients
who require, and those who do not require, more intensive treatment
regimes.
The successful development and assessment of new DLBCL drugs by the
pharmaceutical industry continues to require the accurate classification
of tumour sub-types. As one example, the Oxford University researchers are
currently collaborating with the UK REMoDL-B Clinical Trial Management
Group15 to explore the use of FOXP1 and its isoforms as markers
of a potential response to the proteasome inhibitor Bortezomib in DLBCL.
Sources to corroborate the impact
- Alizadeh AA, Eisen MB, Davis RE, Ma C, Lossos IS, et al. Distinct
types of diffuse large B-cell lymphoma identified by gene expression
profiling. Nature. 403: 503-511(2000).
Available at http://www.nature.com/nature/journal/v403/n6769/full/403503a0.html (accessed 2013)
The description of a gene expression
profiling study reporting two distinct forms of DLBCL, namely
germinal centre B-like DLBCL and activated B-like DLBCL. Germinal
centre B-like was associated with improved survival.
- Shaffer AL, Rosenwald A, Staudt LM. Lymphoid malignancies: the dark
side of B-cell differentiation. Nat Rev Immunol. 2: 920-32
(2002). doi:10.1038/nri953
Available at
http://www.nature.com/nri/journal/v2/n12/pdf/nri953.pdf (accessed 2013)
Gene expression profiling identifying the
FOXP1 transcript as being highly expressed in activated B-cell
subtype of DLBCL.
- Ballabio E, et al. Comparison of Choi and Hans algorithmns by
immunohistochemistry and quantitative reverse transcriptase-PCR — Letter. Clin Cancer Res. 16: 3805-3806 (2010).
Available at http://clincancerres.aacrjournals.org/content/16/14/3805.full.pdf+html (accessed 2013)
A report describing the correlation between
gene expression profiling and immunohistochemistry for subtyping
patients.
- Nyman H, Jerkeman M, Karjalainen-Linsdberg M-J, Banham AH, Leppa S.
Prognostic impact of activated B-cell focused classification in diffuse
large B-cell lymphoma patients treated with R-CHOP. Mod Path.
22: 1094-1101(2009). doi:10.1038/modpathol.2009.73
Available at http://www.nature.com/modpathol/journal/v22/n8/pdf/modpathol200973a.pdf (accessed 2013).
Paper reporting the identification of a
panel of antibodies that enable the identification of subtyes of
DLBCL using immunocytochemical staining techniques. Emphasis is
placed on the FOXP1 and MUM-1 proteins as markers of activated
B-cell derived DLBCL, with their expression linked to significant
inferior failure-free survival.
- Copie-Bergman C, et al. Immunofluorescence in situ hybridisation index
predicts survival in patients with diffuse large B-cell lymphoma treated
with R-CHOP: a GELA study. J Clin Oncol. 27: 5573-79 (2009).
doi: 10.1200/JCO.2009.22.7058
Available at http://jco.ascopubs.org/content/27/33/5573.full.pdf+html (accessed 2013).
A report from two clinical trials
describing the importance of using immunohistochemical labelling for
FOXP1 combined with in situ hybridisation detecting the BCL2, BCL6
and c-MYC oncogenes to predict survival in elderly patients treated
with R-CHOP.
- Thieblemont C, Briere J, Mounier N, et al The germinal
center/activated B-cell subclassification has a prognostic impact for
response to salvage therapy in relapsed/refractory diffuse large B-cell
Lymphoma: A Bio-CORAL study. J Clin Oncol. 29: 4079-4087 (2011).
doi: 10.1200/JCO.2011.35.4423.
Available at http://jco.ascopubs.org/content/29/31/4079.full.pdf+html (accessed 2013)
Paper linking FOXP1 protein expression with
inferior survival in patients with activated B-cell DLBCL.
- Visco C, Li Y, Xu-Monette ZY, Miranda RN, Green TM, et al.
Comprehensive gene expression profiling and immunohistochemical studies
support application of immunophenotypic algorithm for molecular subtype
classification in diffuse large B-cell lymphoma: a report from the
International DLBCL Rituximab-CHOP Consortium Program Study. Leukemia.
26: 2103-13 (2012). doi: 10.1038/leu.2012.83. Available at
http://www.nature.com/leu/journal/v26/n9/pdf/leu201283a.pdf (accessed 2013).
A publication from the International DLBCL
Rituximab-CHOP Consortium Program Study in which FOXP1 was reported
to be one of the three significant molecules for predicting outcome
in DLBCL.
-
http://www.abdserotec.com/product/jc12-anti-foxp1-antibody-mca2485t.html (accessed 2013)
An example of a website from a company
commercialising the JC12 antibody.
- Letter from Dr Andrew Davies, Honorary Consultant Medical Oncology,
Cancer Services Division, University of Southampton. Letter kept on
file, available on request. A letter from Dr Andrew Davies
(member of the lead centre in the study) to Professor Banham for the
REMoDL-B study.